Final ID: P3117
Association of Body Roundness Index (BRI) with Left Ventricular Mass and Geometry: The Framingham Heart Study
Abstract Body: INTRODUCTION: Body roundness index (BRI) is a metric of body shape incorporating both girth (waist circumference, WC) and height (HT), where BRI=364.2 – 365.5*SQRT(1- (WC/(π*HT))2). In contrast to body mass index (BMI) which does not account for body shape, BRI may be better able to identify adiposity. Increased left ventricular mass (LVM) indexed to body size predicts excess cardiovascular morbidity and mortality, but it is not clear whether indexation to HT or powers of HT, or to body surface area (BSA) are optimal. We sought to determine whether there is association between BRI and various methods of LVM indexation.
METHODS: 1764 members (944 women) of the Framingham Offspring cohort underwent cardiac magnetic resonance (CMR). Participants were divided into sex-specific tertiles of BRI, then a “referent group” without prevalent CVD, wall-motion abnormalities on CMR, or any history of hypertension was identified. We used sex-specific ANCOVA to test for linear trend across BRI tertiles for LVM and LVM indexed to HT, HT2.7, BSA, and total body weight (WT). We further investigated two measures of concentricity (“LV geometry”), as high concentricity is associated with excess morbidity. Relative wall thickness (RWT) was LV wall thickness/chamber diameter, Mass-volume ratio (MVR) was LVM/ end-diastolic volume.
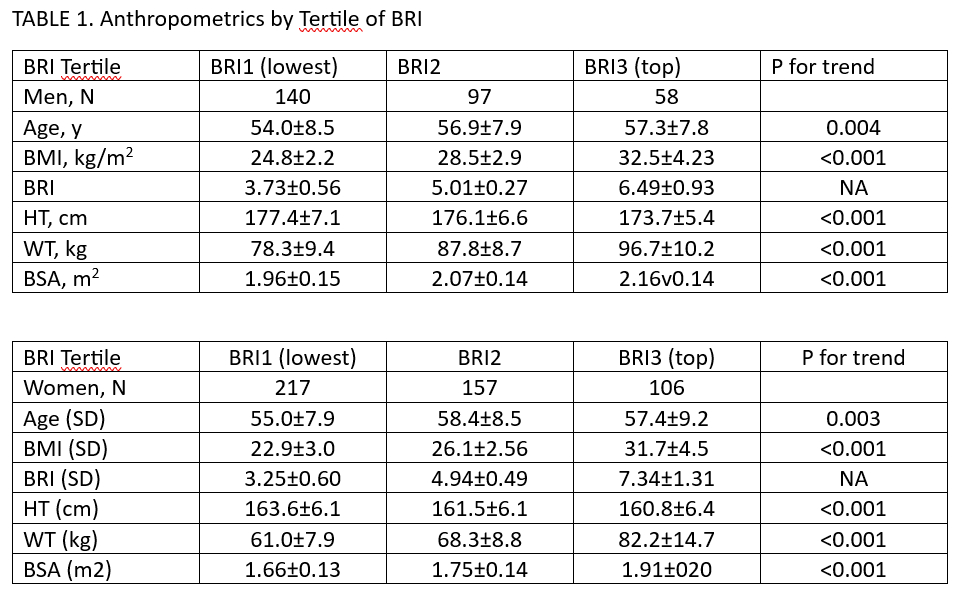
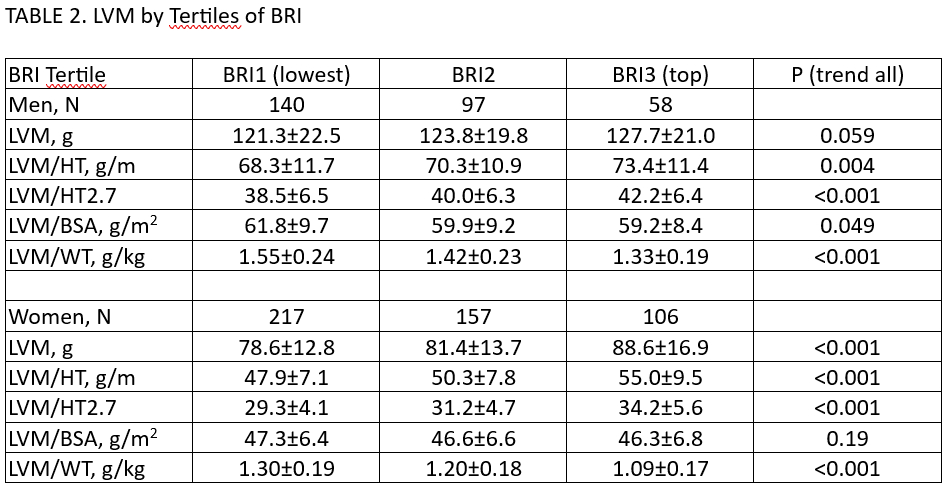
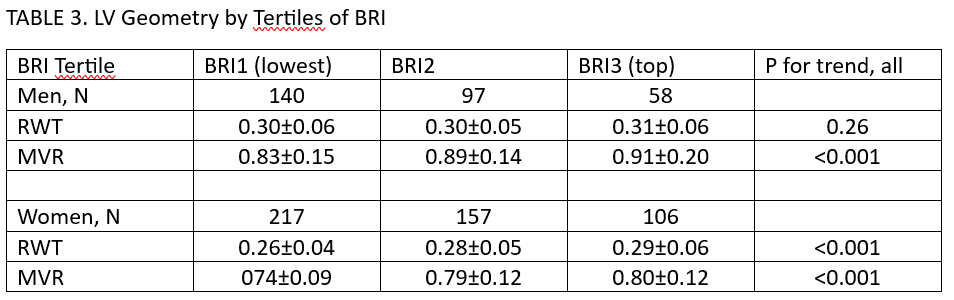
RESULTS: The proportion of Offspring meeting Referent criteria (N=775, 57% women) decreased with greater BRI for each sex; Table 1. Table 2 shows that LVM and LVM indexed to HT or HT2.7 increased with greater BRI, significantly for all except LVM in men. LVM/BSA was not different across tertiles of BRI among women, and decreased minimally (by <3g/m2) in men (p=0.049). LVM/WT decreased markedly with higher BRI in both sexes. RWT did not differ across BRI tertiles in men, but increased among women. MVR increased with greater BRI in both sexes (Table 3).
CONCLUSIONS: LVM indexed to BSA is largely indifferent to BRI, but HT-indexed LVM increases, and LVM/WT decreases with greater BRI category. These results may suggest that HT indexation, which does not account for WT, may be “under adjustment”. However, simply indexing to WT may also be inappropriate, if the allometric relationship between LVM and body mass is dependent on the type of mass (i.e. fat vs non-fat mass). It remains to be determined which method of LVM indexation is best predictive of incident cardiovascular and overall morbidity and mortality.
METHODS: 1764 members (944 women) of the Framingham Offspring cohort underwent cardiac magnetic resonance (CMR). Participants were divided into sex-specific tertiles of BRI, then a “referent group” without prevalent CVD, wall-motion abnormalities on CMR, or any history of hypertension was identified. We used sex-specific ANCOVA to test for linear trend across BRI tertiles for LVM and LVM indexed to HT, HT2.7, BSA, and total body weight (WT). We further investigated two measures of concentricity (“LV geometry”), as high concentricity is associated with excess morbidity. Relative wall thickness (RWT) was LV wall thickness/chamber diameter, Mass-volume ratio (MVR) was LVM/ end-diastolic volume.
RESULTS: The proportion of Offspring meeting Referent criteria (N=775, 57% women) decreased with greater BRI for each sex; Table 1. Table 2 shows that LVM and LVM indexed to HT or HT2.7 increased with greater BRI, significantly for all except LVM in men. LVM/BSA was not different across tertiles of BRI among women, and decreased minimally (by <3g/m2) in men (p=0.049). LVM/WT decreased markedly with higher BRI in both sexes. RWT did not differ across BRI tertiles in men, but increased among women. MVR increased with greater BRI in both sexes (Table 3).
CONCLUSIONS: LVM indexed to BSA is largely indifferent to BRI, but HT-indexed LVM increases, and LVM/WT decreases with greater BRI category. These results may suggest that HT indexation, which does not account for WT, may be “under adjustment”. However, simply indexing to WT may also be inappropriate, if the allometric relationship between LVM and body mass is dependent on the type of mass (i.e. fat vs non-fat mass). It remains to be determined which method of LVM indexation is best predictive of incident cardiovascular and overall morbidity and mortality.
More abstracts on this topic:
A combined approach of cardiac magnetic resonance and CardioMEMS to assess right ventricular dysfunction during exercise in HFpEF-PH
Bekhuis Youri, Bogaert Jan, La Gerche Andre, Claessen Guido, Janssens Stefan, Droogne Walter, Rosseel Thomas, Barrios Leticia, Verwerft Jan, Timmermans Philippe, Trenson Sander, Dresselaers Tom
A Clinical Trial of Healthy Food Subsidies and Behavioral Interventions to Increase Fruit and Vegetable Purchasing in an Online StoreHua Sophia, Klaiman Tamar, Dixon Erica, Volpp Kevin, Putt Mary, Coratti Samantha, White Jenna, Hossain Mohammad, Posner Hannah, Wang Erkuan, Zhu Jingsan, John Aileen