Final ID: P3145
Variation in Cerebrovascular Disease Mortality among Asian American Ethnic Subgroups
Abstract Body:
Introduction: While cerebrovascular disease is the 5th leading cause of death in the United States, there is limited knowledge about cerebrovascular disease mortality in Asian Americans. Asian Americans are more likely to experience severe ischemic strokes compared to non-Hispanic Whites. This study examines the variability in cerebrovascular disease mortality among disaggregated Asian Americans from 2012 to 2022.
Methods: We analyzed US death certificate data for cerebrovascular disease among non-Hispanic Asian American subgroups (Chinese, Filipino, Asian Indian, Japanese, Korean, and Vietnamese) and non-Hispanic White (NHW) Americans from 2012 to 2022. We calculated age-standardized mortality rates (ASMR), average annual percent change (AAPC) of ASMR using Joinpoint regression analysis, and proportional mortality ratios of cerebrovascular disease.
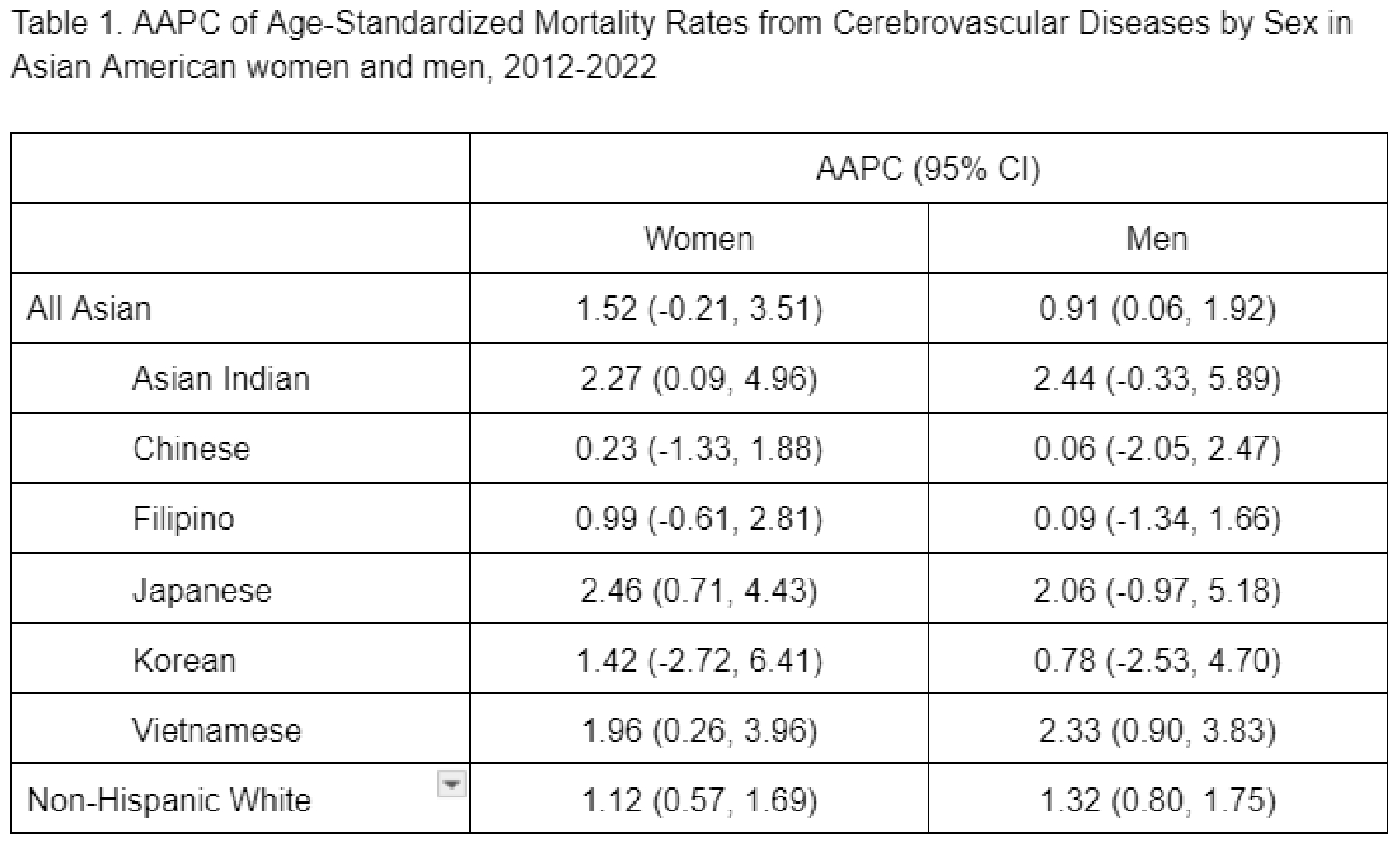
Results: Among 672,654 non-Hispanic Asian American and 268,574,419 non-Hispanic White deaths from all causes, ASMR from cerebrovascular disease significantly increased in Asian American men in aggregate, Asian Indian women, Japanese women, Vietnamese men and women, and non-Hispanic White men and women from 2012 to 2022, and remained stagnant in Asian American women, Asian Indian men, Chinese men and women, Filipino men and women, Japanese men, Korean men and women (Table 1). The highest ASMR from cerebrovascular disease in 2022 among Asian American subgroups was in Vietnamese women (37 per 100,000) and men (48 per 100,000). In 2022, cerebrovascular disease represented 7.1% to 9.5% of deaths of Asian American women and 5.1% to 7.6% of deaths of Asian American men. Relative to the general U.S. population, proportional mortality ratios for cerebrovascular disease ranged from 1.18 in Korean American women to 1.63 in Vietnamese American women and 1.21 in Japanese American men to 1.87 in Vietnamese American men.
Conclusion: The increasing mortality of cerebrovascular disease among disaggregated Asian Americans over the past decade, especially surrounding the COVID-19 pandemic, highlights the need for directed treatment and prevention efforts to address cerebrovascular disease in these diverse populations.
Introduction: While cerebrovascular disease is the 5th leading cause of death in the United States, there is limited knowledge about cerebrovascular disease mortality in Asian Americans. Asian Americans are more likely to experience severe ischemic strokes compared to non-Hispanic Whites. This study examines the variability in cerebrovascular disease mortality among disaggregated Asian Americans from 2012 to 2022.
Methods: We analyzed US death certificate data for cerebrovascular disease among non-Hispanic Asian American subgroups (Chinese, Filipino, Asian Indian, Japanese, Korean, and Vietnamese) and non-Hispanic White (NHW) Americans from 2012 to 2022. We calculated age-standardized mortality rates (ASMR), average annual percent change (AAPC) of ASMR using Joinpoint regression analysis, and proportional mortality ratios of cerebrovascular disease.
Results: Among 672,654 non-Hispanic Asian American and 268,574,419 non-Hispanic White deaths from all causes, ASMR from cerebrovascular disease significantly increased in Asian American men in aggregate, Asian Indian women, Japanese women, Vietnamese men and women, and non-Hispanic White men and women from 2012 to 2022, and remained stagnant in Asian American women, Asian Indian men, Chinese men and women, Filipino men and women, Japanese men, Korean men and women (Table 1). The highest ASMR from cerebrovascular disease in 2022 among Asian American subgroups was in Vietnamese women (37 per 100,000) and men (48 per 100,000). In 2022, cerebrovascular disease represented 7.1% to 9.5% of deaths of Asian American women and 5.1% to 7.6% of deaths of Asian American men. Relative to the general U.S. population, proportional mortality ratios for cerebrovascular disease ranged from 1.18 in Korean American women to 1.63 in Vietnamese American women and 1.21 in Japanese American men to 1.87 in Vietnamese American men.
Conclusion: The increasing mortality of cerebrovascular disease among disaggregated Asian Americans over the past decade, especially surrounding the COVID-19 pandemic, highlights the need for directed treatment and prevention efforts to address cerebrovascular disease in these diverse populations.
More abstracts on this topic:
Analysis of Racial Disparities in the Training Path to Cardiology: Trends from 2012 to 2022
Gopal Jay, Rahafrooz Maryam, Chan Nathan, Gopal Devraj, Kepler Joshua, Ren Junling, Gopal Indulekha, Joseph Jacob
A Bridge from Sweet to Sour: A Case of Recurrent Myocardial Stunning in Diabetic KetoacidosisSatish Vikyath, Pargaonkar Sumant, Slipczuk Leandro, Schenone Aldo, Maliha Maisha, Chi Kuan Yu, Sunil Kumar Sriram, Borkowski Pawel, Vyas Rhea, Rodriguez Szaszdi David Jose Javier, Kharawala Amrin, Seo Jiyoung