Final ID: P1014
The associations of financial barriers to dental health care with incident cardiovascular disease and dementia: a longitudinal analysis in the All of Us cohort
Abstract Body: Introduction: Though poor oral health is linked to elevated risk of later-life cardiovascular disease (CVD) and Alzheimer’s Disease and Related Dementias (ADRD) via systemic inflammation, the impact of financial barriers to oral care on CVD and ADRD incidence remains unquantified.
Hypothesis: We hypothesized that older adults reporting financial barriers to oral care -particularly women, people marginalized due to racial/ethnic identity, or with periodontitis - have elevated risk for CVD and ADRD.
Methods: We used data from All of Us participants aged at least 55 years (N=65,770, 77.2% Non-Hispanic White, 57.9% women). Our primary exposure was self-reported difficulty accessing oral care due to cost within the past year, defined as yes or no. We identified congestive heart failure (CHF), cerebrovascular accident (CVA), myocardial infarction (MI) and ADRD outcomes in linked electronic health records. Using Cox proportional hazards models, we estimated associations of difficulty accessing dental care with each outcome. We assessed heterogeneity by gender, racial/ethnic identity, and prevalent periodontitis diagnosis. We estimated the population attributable fractions (PAF) of each outcome associated with difficulty accessing oral care using national prevalence estimates.
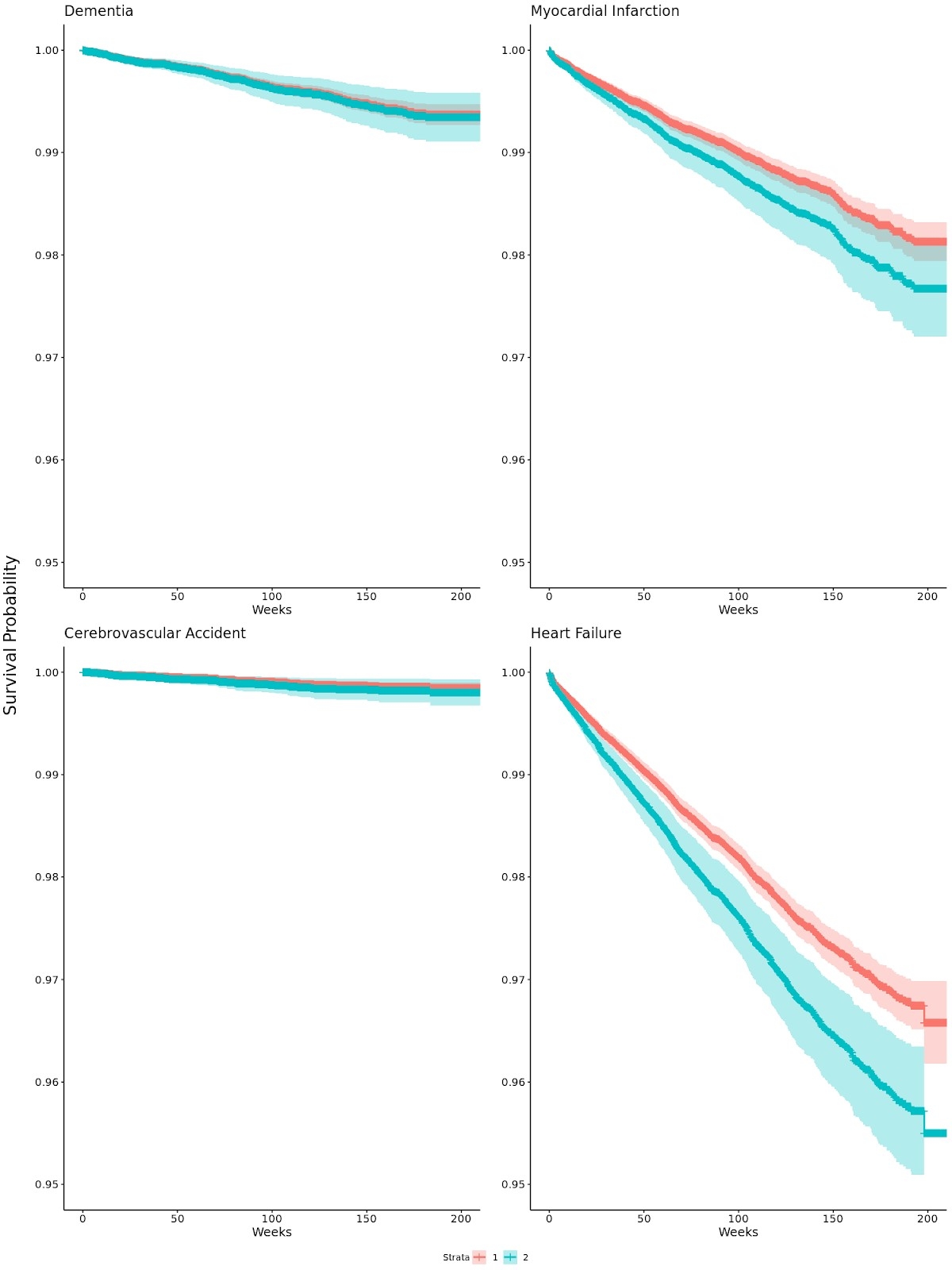
Results: Participants who reported difficulty affording oral care had a higher incidence of CVA (adjusted HR=1.72; 95% CI: 0.72, 3.86) and CHF (HR=1.22; 95% CI: 1.01, 1.47). Estimated effects on MI (HR=1.11; 95% CI: 0.85, 1.44) and ADRD (HR=1.02; 95% CI: 0.61, 1.69) were not robust to adjustment for demographic, health behavioral, and clinical confounders. We did not observe differences in these associations by race/ethnicity, gender, or periodontitis. The estimated PAFs suggest that eliminating financial barriers to oral care could, over three years, prevent 9% of incident stroke, 4% of MI, 6% of CHF, and 4% of ADRD.
Conclusion: Addressing financial barriers to needed oral care remains an unrealized policy target for CVD and ADRD prevention.
Hypothesis: We hypothesized that older adults reporting financial barriers to oral care -particularly women, people marginalized due to racial/ethnic identity, or with periodontitis - have elevated risk for CVD and ADRD.
Methods: We used data from All of Us participants aged at least 55 years (N=65,770, 77.2% Non-Hispanic White, 57.9% women). Our primary exposure was self-reported difficulty accessing oral care due to cost within the past year, defined as yes or no. We identified congestive heart failure (CHF), cerebrovascular accident (CVA), myocardial infarction (MI) and ADRD outcomes in linked electronic health records. Using Cox proportional hazards models, we estimated associations of difficulty accessing dental care with each outcome. We assessed heterogeneity by gender, racial/ethnic identity, and prevalent periodontitis diagnosis. We estimated the population attributable fractions (PAF) of each outcome associated with difficulty accessing oral care using national prevalence estimates.
Results: Participants who reported difficulty affording oral care had a higher incidence of CVA (adjusted HR=1.72; 95% CI: 0.72, 3.86) and CHF (HR=1.22; 95% CI: 1.01, 1.47). Estimated effects on MI (HR=1.11; 95% CI: 0.85, 1.44) and ADRD (HR=1.02; 95% CI: 0.61, 1.69) were not robust to adjustment for demographic, health behavioral, and clinical confounders. We did not observe differences in these associations by race/ethnicity, gender, or periodontitis. The estimated PAFs suggest that eliminating financial barriers to oral care could, over three years, prevent 9% of incident stroke, 4% of MI, 6% of CHF, and 4% of ADRD.
Conclusion: Addressing financial barriers to needed oral care remains an unrealized policy target for CVD and ADRD prevention.
More abstracts on this topic:
6-Nitrodopamine potentiates the positive chronotopic and inotropic effect induced by noradrenaline in the rat isolated heart
Lima Antonio, Sobanski Joao Fernando, Antunes Edson, De Nucci Gilberto
A Case of Steroid-Refractory Immune-checkpoint-inhibitor Induced Myocarditis Responsive to Mycophenolate and Anti-thymocyte globulinDabdoub Jorge, Wilson Michael, Gottbrecht Matthew, Salazar Ryan, Shih Jeffrey