Final ID: MP70
The Burden of Protein-Energy Malnutrition Mortality in Older Adults by County, Race, and Ethnicity in the USA,2000-19: A Systematic Analysis of Health Disparities
Abstract Body: Importance: Older adults have a higher malnutrition risk due to aging, chronic diseases, and social vulnerabilities. Understanding malnutrition mortality trends across racial/ethnic groups helps guide interventions to reduce health disparities and improve quality of life.
Objectives: Estimate malnutrition mortality rates among older adults (ages 65-74 and ≥75) nationally and by county for racial/ethnic groups.
Design/Setting: Analysis of National Vital Statistics System death registration (2000-2019), using small-area estimation to adjust for misclassification of race/ethnicity on death certificates.
Exposure: Race/ethnicity (American Indian/Alaska Native (AIAN), Asian, Black, Latino, White) and county, mapped to temporally stable geographical units.
Main Outcomes and Measures: Deaths due to malnutrition (ICD codes E40-E46.9, E64).
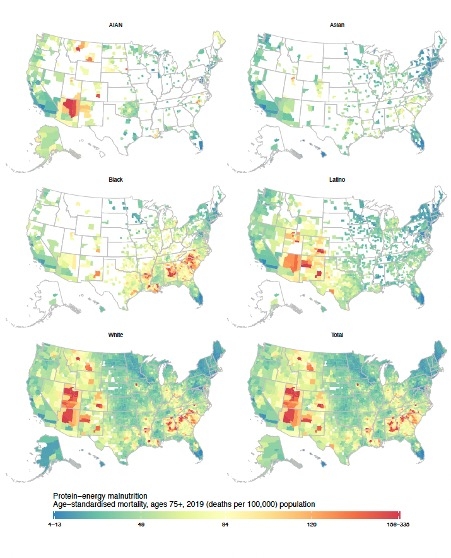
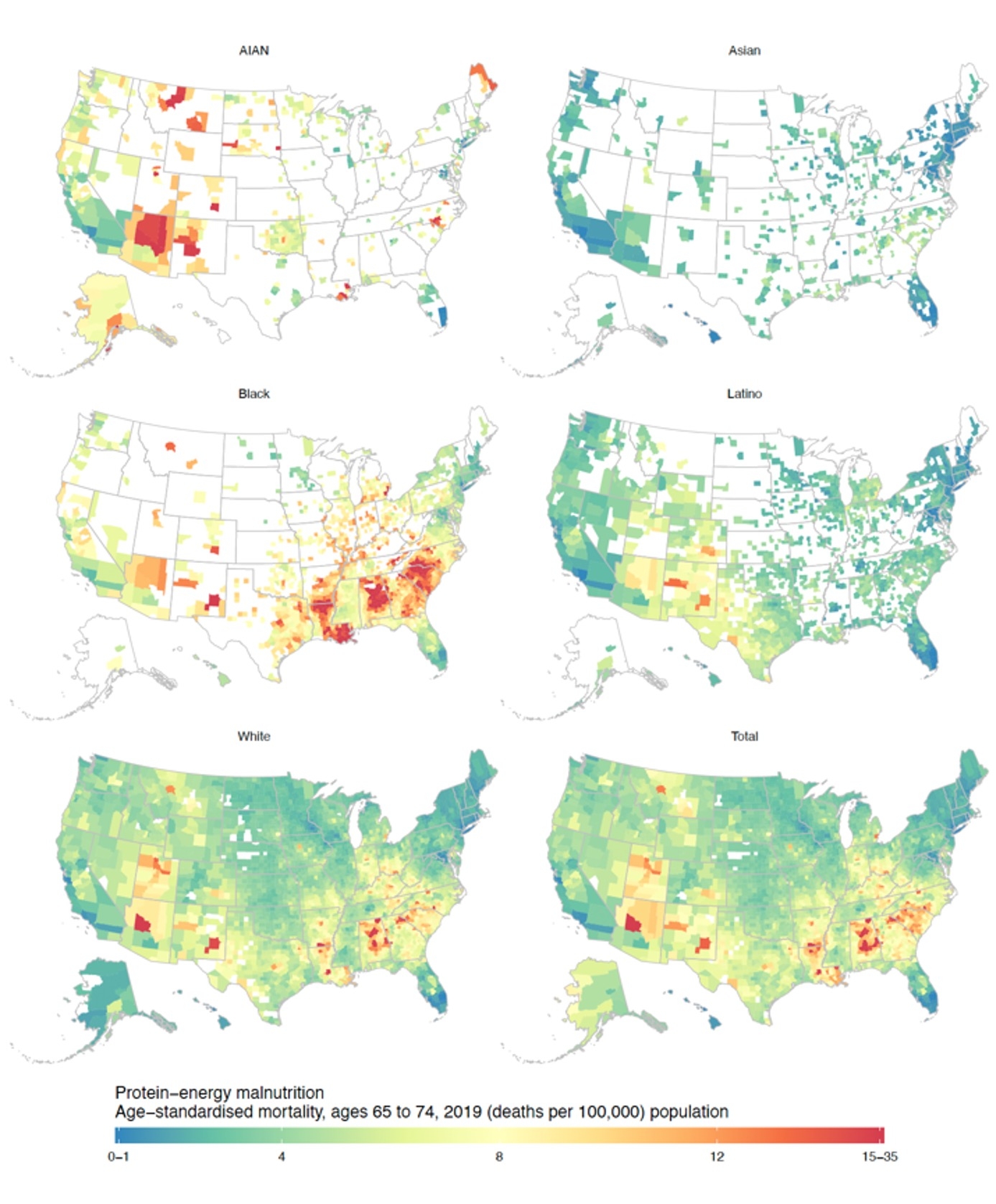
Results: In 2019, adults aged ≥75 had the highest malnutrition mortality rate (49.2 per 100,000) compared to those aged 65-74 (4.6 per 100,000). Between 2000-2019, mortality increased for both ≥75 (19.5 to 49.2 per 100,000) and 65-74 (2.2 to 4.6 per 100,000). The Black population consistently had the highest malnutrition mortality rates (2019: ≥75: 60.8 per 100,000; 65-74: 7.7 per 100,000), followed by AIAN, White, Latino, and Asian populations.
County-level analysis showed wide mortality variations for those ≥75 (4.9–308.9 per 100,000) and 65-74 (1.5–24.0 per 100,000). The South, particularly for Black individuals, was most affected, with rates of 0.6–27.9 per 100,000 (65-74) and 4.4–208.3 per 100,000 (≥75), with 66.2% of counties located in southern metro areas. For AIAN, mortality ranged from 0.6–34.9 per 100,000 (65-74) and 5.5–254.7 per 100,000 (≥75), with 75% in Rocky Mountains' metro areas. White individuals had rates of 0.4–25.0 per 100,000 (65-74) and 5.2–334.9 per 100,000 (≥75), mainly in nonmetro-Southern counties. Latino mortality ranged from 0.4–13.2 per 100,000 (65-74) and 4.2–173.1 per 100,000 (≥75), mostly in Rocky Mountains’ nonmetro areas, while Asian rates were 0.4–7.3 per 100,000 (65-74) and 4.4–141.5 per 100,000 (≥75), mainly in Rocky Mountains’ metro areas.
Conclusions and Relevance Malnutrition mortality among older adults increased over the study period, particularly for those aged ≥75 in Southeastern counties. The variation across geography, age, race, and ethnicity indicates the need for targeted malnutrition screening, treatment, and nutritional interventions and policies for older adults.
Objectives: Estimate malnutrition mortality rates among older adults (ages 65-74 and ≥75) nationally and by county for racial/ethnic groups.
Design/Setting: Analysis of National Vital Statistics System death registration (2000-2019), using small-area estimation to adjust for misclassification of race/ethnicity on death certificates.
Exposure: Race/ethnicity (American Indian/Alaska Native (AIAN), Asian, Black, Latino, White) and county, mapped to temporally stable geographical units.
Main Outcomes and Measures: Deaths due to malnutrition (ICD codes E40-E46.9, E64).
Results: In 2019, adults aged ≥75 had the highest malnutrition mortality rate (49.2 per 100,000) compared to those aged 65-74 (4.6 per 100,000). Between 2000-2019, mortality increased for both ≥75 (19.5 to 49.2 per 100,000) and 65-74 (2.2 to 4.6 per 100,000). The Black population consistently had the highest malnutrition mortality rates (2019: ≥75: 60.8 per 100,000; 65-74: 7.7 per 100,000), followed by AIAN, White, Latino, and Asian populations.
County-level analysis showed wide mortality variations for those ≥75 (4.9–308.9 per 100,000) and 65-74 (1.5–24.0 per 100,000). The South, particularly for Black individuals, was most affected, with rates of 0.6–27.9 per 100,000 (65-74) and 4.4–208.3 per 100,000 (≥75), with 66.2% of counties located in southern metro areas. For AIAN, mortality ranged from 0.6–34.9 per 100,000 (65-74) and 5.5–254.7 per 100,000 (≥75), with 75% in Rocky Mountains' metro areas. White individuals had rates of 0.4–25.0 per 100,000 (65-74) and 5.2–334.9 per 100,000 (≥75), mainly in nonmetro-Southern counties. Latino mortality ranged from 0.4–13.2 per 100,000 (65-74) and 4.2–173.1 per 100,000 (≥75), mostly in Rocky Mountains’ nonmetro areas, while Asian rates were 0.4–7.3 per 100,000 (65-74) and 4.4–141.5 per 100,000 (≥75), mainly in Rocky Mountains’ metro areas.
Conclusions and Relevance Malnutrition mortality among older adults increased over the study period, particularly for those aged ≥75 in Southeastern counties. The variation across geography, age, race, and ethnicity indicates the need for targeted malnutrition screening, treatment, and nutritional interventions and policies for older adults.
More abstracts on this topic:
Activin Type IIA Receptor Inhibition Decreases Atrial Fibrillation Inducibility In Mice Via a Smurf1-Connexin43 Mechanism
Castro Claire, Lee Se-jin, Ellinor Patrick, Rosenzweig Anthony, Roh Jason, Bapat Aneesh, Hobson Ryan, Yu Andy, Li Haobo, Xiao Chunyang, Xia Peng, Yeri Ashish, Yu Paul
4D Flow MRI Evaluation of Cardiovascular Risk-Related Alterations in Heart-Brain Hemodynamics in Cognitively Healthy Aging AdultsNajafi Anahita, Rogalski Emily, Jarvis Kelly, Richter Adam, Lytchakov Anna, Benson Theresa, Jin Ning, Davids Rachel, Schnell Susanne, Ragin Ann, Weintraub Sandra