Final ID: P2086
Sex and Racial Differences in Prescription Patterns to Guideline-directed Medical Therapy Among STEMI Patients.
Abstract Body:
Background: ST-elevation myocardial infarction (STEMI) is associated with serious complications and mortality. Percutaneous coronary intervention (PCI) is the principal reperfusion strategy for STEMI patients, followed by pharmacologic therapy to prevent recurrent cardiovascular (CV) events. The American Heart Association (AHA) and American College of Cardiology (ACC) recommend the use of guideline directed medical therapy (GDMT) prescribed at hospital discharge following a STEMI. Given the well-described sex and racial differences in the adherence to pharmacologic therapies, this study aimed to assess whether sex and racial differences also exist in GDMT prescribing patterns in STEMI patients at hospital discharge.
Methods: Analyses were performed on 734 STEMI patients (176 females, 558 males; 78.5% white) that presented to two urban emergency departments between January 1, 2022, and March 31, 2024 and underwent PCI during admission. Discharge prescriptions for GDMT based on AHA/ACC guidelines (Aspirin, P2Y12 inhibitors, β-blockers (BBs), angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs), and statins) were compared by sex and race using chi-square tests of association. Given that physicians commonly only prescribe ACEIs/ARBS when ejection fraction (EF) is low, sub-analyses were run on patients with EF <50%.
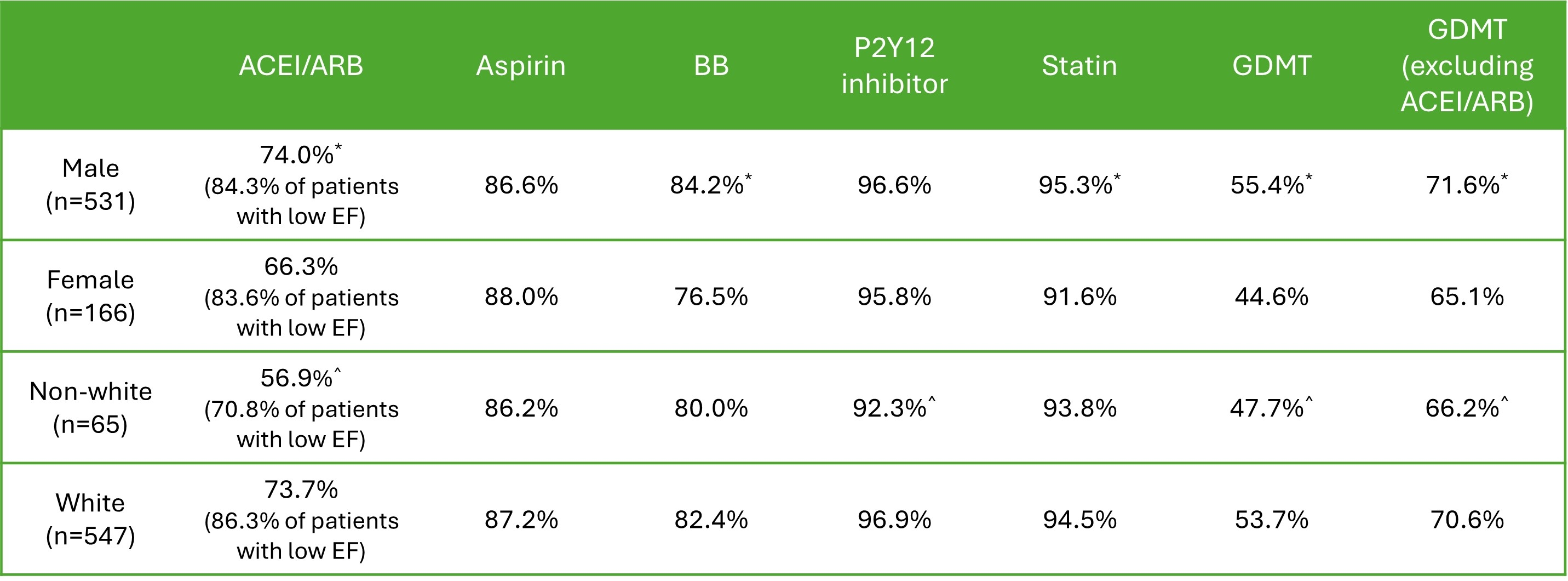
Results: Table 1 shows differences in GDMT prescribed at discharge by sex and race categories. Among patients with successful PCI, 52.8% were prescribed all five GDMT and 70.0% were prescribed four secondary prevention medications (Aspirin, P2Y12 inhibitors, BBs, statins). Males were more likely to be prescribed all five GDMT at discharge compared to females (55.4 vs. 44.6%). The greatest difference in medication class prescribed between sexes was for BBs (80.1 vs. 72.2%). Racial disparities were also noted, as white patients were more likely to receive all five GDMT at discharge compared to non-white patients (53.7 vs. 47.7%). The greatest difference in medication class prescribed between white and non-white patients was for ACEI/ARBs (63.1 vs. 49.3%). Racial differences remained significant when only assessing patients with low EF (86.3 vs. 70.8% on ACEI/ARB).
Conclusion: Optimal secondary prevention medications are effective in reducing the risk of repeat CV events. Strategies are needed to address sex and racial disparities in GDMT prescribing patterns to achieve AHA/ACC guidelines and improve patient outcomes.
Background: ST-elevation myocardial infarction (STEMI) is associated with serious complications and mortality. Percutaneous coronary intervention (PCI) is the principal reperfusion strategy for STEMI patients, followed by pharmacologic therapy to prevent recurrent cardiovascular (CV) events. The American Heart Association (AHA) and American College of Cardiology (ACC) recommend the use of guideline directed medical therapy (GDMT) prescribed at hospital discharge following a STEMI. Given the well-described sex and racial differences in the adherence to pharmacologic therapies, this study aimed to assess whether sex and racial differences also exist in GDMT prescribing patterns in STEMI patients at hospital discharge.
Methods: Analyses were performed on 734 STEMI patients (176 females, 558 males; 78.5% white) that presented to two urban emergency departments between January 1, 2022, and March 31, 2024 and underwent PCI during admission. Discharge prescriptions for GDMT based on AHA/ACC guidelines (Aspirin, P2Y12 inhibitors, β-blockers (BBs), angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs), and statins) were compared by sex and race using chi-square tests of association. Given that physicians commonly only prescribe ACEIs/ARBS when ejection fraction (EF) is low, sub-analyses were run on patients with EF <50%.
Results: Table 1 shows differences in GDMT prescribed at discharge by sex and race categories. Among patients with successful PCI, 52.8% were prescribed all five GDMT and 70.0% were prescribed four secondary prevention medications (Aspirin, P2Y12 inhibitors, BBs, statins). Males were more likely to be prescribed all five GDMT at discharge compared to females (55.4 vs. 44.6%). The greatest difference in medication class prescribed between sexes was for BBs (80.1 vs. 72.2%). Racial disparities were also noted, as white patients were more likely to receive all five GDMT at discharge compared to non-white patients (53.7 vs. 47.7%). The greatest difference in medication class prescribed between white and non-white patients was for ACEI/ARBs (63.1 vs. 49.3%). Racial differences remained significant when only assessing patients with low EF (86.3 vs. 70.8% on ACEI/ARB).
Conclusion: Optimal secondary prevention medications are effective in reducing the risk of repeat CV events. Strategies are needed to address sex and racial disparities in GDMT prescribing patterns to achieve AHA/ACC guidelines and improve patient outcomes.
More abstracts on this topic:
A Novel ECG Time-Frequency Eyeball Method for Robust Detection of Myocardial Infarction from Single-Channel ECG: A Preclinical Study
Alavi Rashid, Li Jiajun, Dai Wangde, Matthews Ray, Pahlevan Niema, Kloner Robert, Gharib Morteza
Assessing Coronary Artery Disease Severity: Leveraging Inflammatory Markers As a Prognostic IndicatorsTurnbull Scott, Dugal Jasmine, Gill Randeep, Wang Shawn, Cross Chad, Mubder Mohamad