Final ID: MP2469
Outpacing Tradition: Conduction System Pacing Demonstrates Superior Outcomes to Biventricular Pacing for HFrEF.
Abstract Body (Do not enter title and authors here): Background
Cardiac resynchronization therapy (CRT) improves outcomes in heart failure patients with reduced ejection fraction (HFrEF) and ventricular dyssynchrony. While biventricular pacing (BVP) is the standard approach, it produces non-physiologic activation and leaves up to one-third of patients as non-responders. Conduction system pacing (CSP)—including His bundle and left bundle branch pacing—offers a more physiologic alternative by engaging native conduction pathways.We conducted a meta-analysis of randomized controlled trials (RCTs) comparing CSP and BVP to assess differences in clinical and echocardiographic outcomes
Methods:
A systematic search of PubMed, Scopus, and Cochrane databases identified 8 RCTs including 477 patients with HFrEF undergoing CRT. Outcomes analyzed included QRS duration, NYHA functional class, left ventricular ejection fraction (LVEF), end-systolic volume (LVESV), pacing threshold, and procedural time. Fixed-effect meta-analyses were performed, and heterogeneity was assessed using the I2 statistic.
Results:
Compared to BVP, CSP significantly improved key resynchronization metrics:
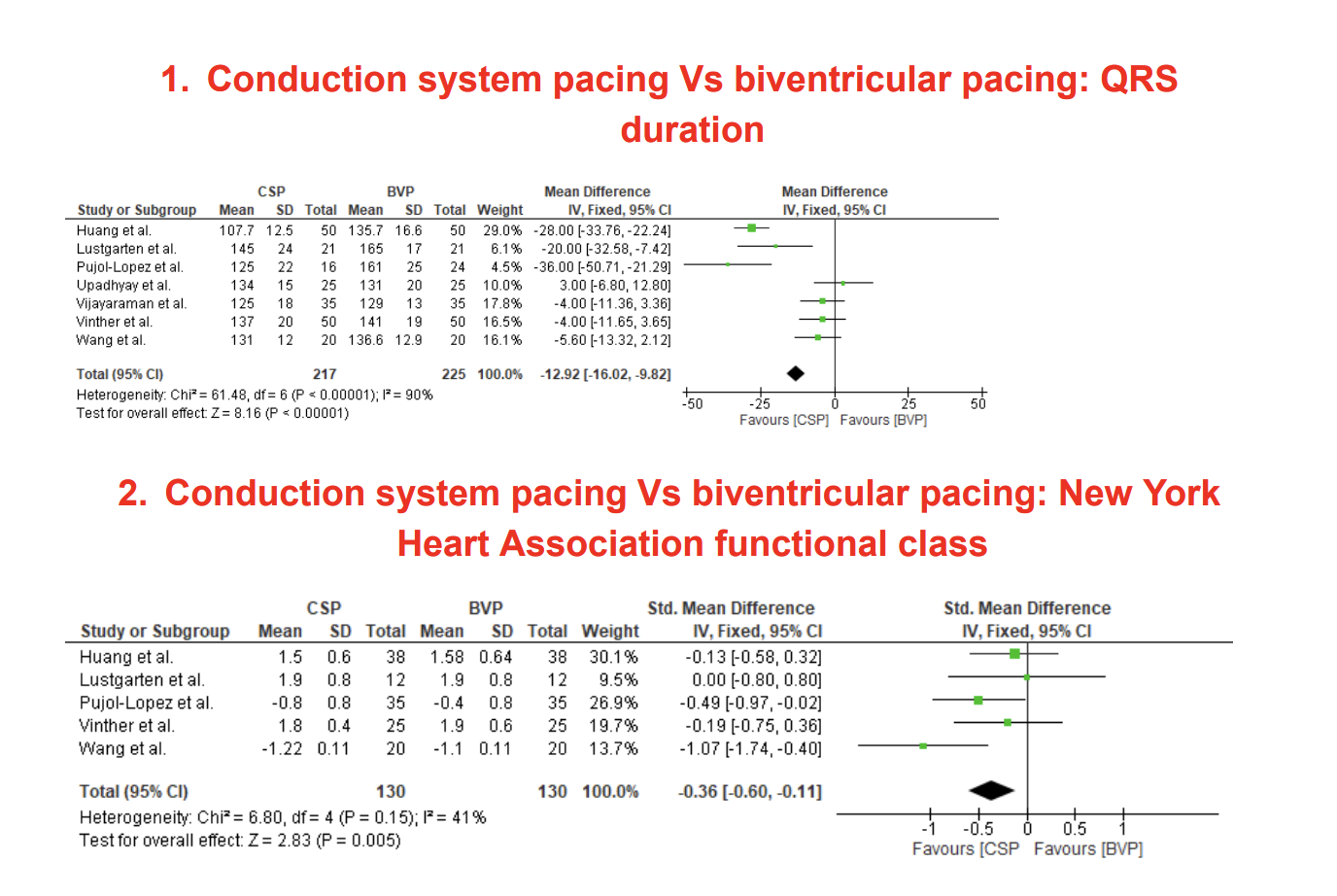
-QRS Duration: CSP shortened QRS more than BVP (MD: -12.92 ms, 95% CI: -16.02 to -9.82, P < 0.00001).
-NYHA Class: Functional status was superior with CSP (SMD: -0.36, 95% CI: -0.60 to -0.11, P = 0.005).
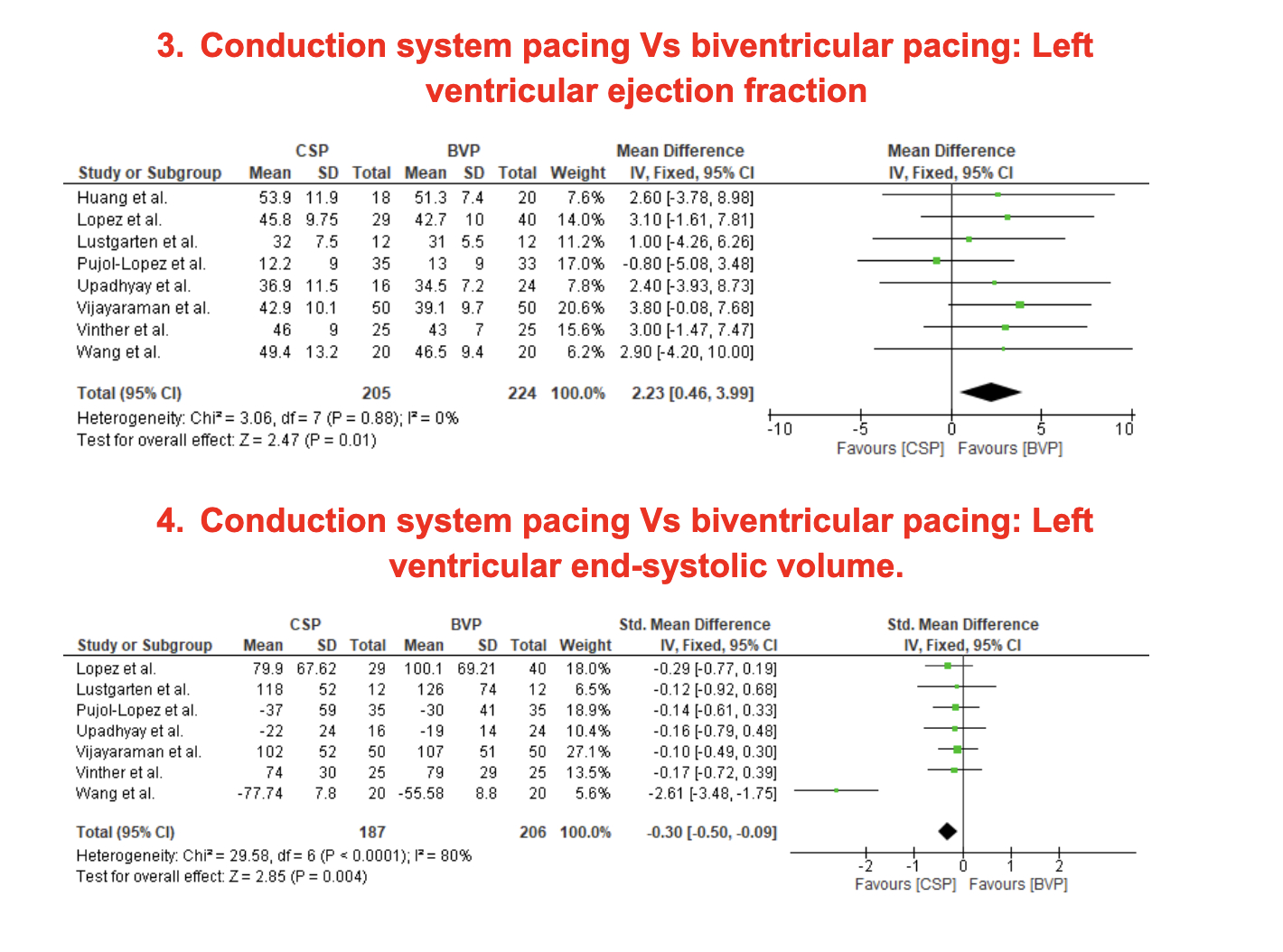
-LVEF: Greater improvement in LVEF with CSP (MD: +2.23%, 95% CI: 0.46 to 3.99, P = 0.01).
-LVESV: CSP led to more favorable reverse remodeling (SMD: -0.30, 95% CI: -0.50 to -0.09, P = 0.004).
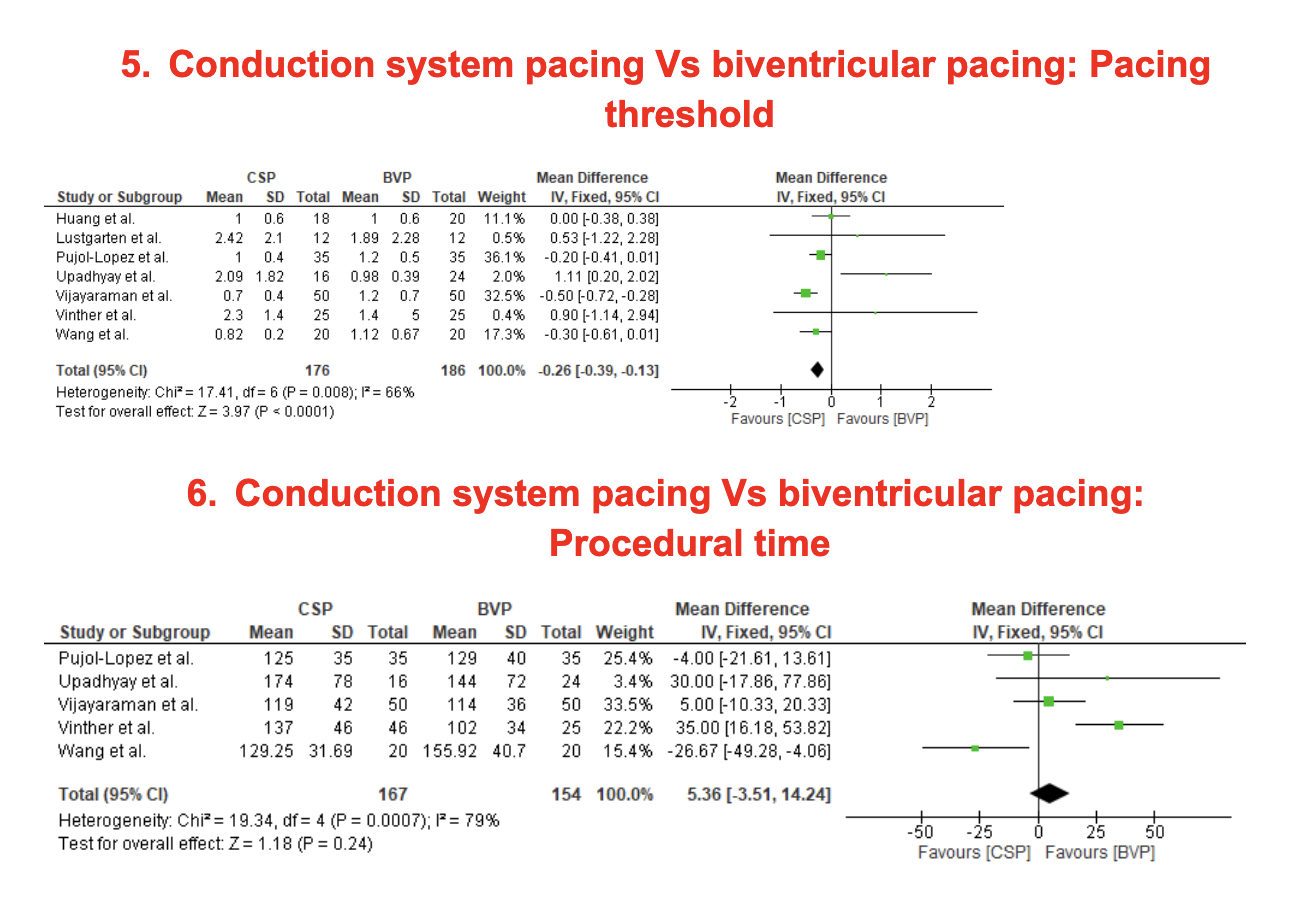
-Pacing Threshold: Lower pacing threshold observed with CSP (MD: -0.26 V, 95% CI: -0.39 to -0.13, P < 0.0001).
-Procedural Time: No significant difference (MD: +5.36 min, 95% CI: -3.51 to 14.24, P = 0.24).
Conclusion
This meta-analysis of randomized trials shows CSP offers superior electrical and clinical outcomes compared to BVP in CRT-eligible HFrEF patients. CSP led to greater QRS narrowing, improved NYHA class, enhanced ejection fraction, and reduced end-systolic volume. Pacing thresholds were lower with CSP, supporting device longevity. Although procedural time was higher, the clinical benefits may outweigh this limitation. These findings support CSP as a promising first-line CRT strategy, warranting broader adoption and further long-term evaluation.
Cardiac resynchronization therapy (CRT) improves outcomes in heart failure patients with reduced ejection fraction (HFrEF) and ventricular dyssynchrony. While biventricular pacing (BVP) is the standard approach, it produces non-physiologic activation and leaves up to one-third of patients as non-responders. Conduction system pacing (CSP)—including His bundle and left bundle branch pacing—offers a more physiologic alternative by engaging native conduction pathways.We conducted a meta-analysis of randomized controlled trials (RCTs) comparing CSP and BVP to assess differences in clinical and echocardiographic outcomes
Methods:
A systematic search of PubMed, Scopus, and Cochrane databases identified 8 RCTs including 477 patients with HFrEF undergoing CRT. Outcomes analyzed included QRS duration, NYHA functional class, left ventricular ejection fraction (LVEF), end-systolic volume (LVESV), pacing threshold, and procedural time. Fixed-effect meta-analyses were performed, and heterogeneity was assessed using the I2 statistic.
Results:
Compared to BVP, CSP significantly improved key resynchronization metrics:
-QRS Duration: CSP shortened QRS more than BVP (MD: -12.92 ms, 95% CI: -16.02 to -9.82, P < 0.00001).
-NYHA Class: Functional status was superior with CSP (SMD: -0.36, 95% CI: -0.60 to -0.11, P = 0.005).
-LVEF: Greater improvement in LVEF with CSP (MD: +2.23%, 95% CI: 0.46 to 3.99, P = 0.01).
-LVESV: CSP led to more favorable reverse remodeling (SMD: -0.30, 95% CI: -0.50 to -0.09, P = 0.004).
-Pacing Threshold: Lower pacing threshold observed with CSP (MD: -0.26 V, 95% CI: -0.39 to -0.13, P < 0.0001).
-Procedural Time: No significant difference (MD: +5.36 min, 95% CI: -3.51 to 14.24, P = 0.24).
Conclusion
This meta-analysis of randomized trials shows CSP offers superior electrical and clinical outcomes compared to BVP in CRT-eligible HFrEF patients. CSP led to greater QRS narrowing, improved NYHA class, enhanced ejection fraction, and reduced end-systolic volume. Pacing thresholds were lower with CSP, supporting device longevity. Although procedural time was higher, the clinical benefits may outweigh this limitation. These findings support CSP as a promising first-line CRT strategy, warranting broader adoption and further long-term evaluation.
More abstracts on this topic:
Mechanical Augmentation of the Failing Heart Results in Improved Intraventricular Synchrony Without Blood Contact
Anstadt Mark, Conley Deborah, Schmitt Benjamin
Improvement in Valvular Regurgitation Severity with Atrioventricular Junction Ablation: Conduction System and Biventricular DevicesKrayem Hussein, Bhardwaj Hem, Trankle Cory, Turlington Jeremy, Kron Jordana, Shepard Richard, Mankad Pranav, Koneru Jayanthi, Ellenbogen Kenneth, Pillai Ajay, Gertz Zachary, Nation Charles, Peddibhotla Bharath, Prabhu Sagar, Shaikh Rafae, Gadela Vaishnavi, Kolominsky Jeffrey, Kontos Michael, Naz Naveed