Final ID: MP869
Percutaneous Valve Implantation in Pulmonary Artery Branches for Severe Pulmonary Regurgitation Secondary to Native Valve Endocarditis
Abstract Body (Do not enter title and authors here): Background
Percutaneous treatment of pulmonary valve disease is a safe and minimally invasive alternative with favorable mid-term outcomes, especially in congenital heart disease. However, feasibility depends on right ventricular outflow tract (RVOT) anatomy, with dilation being the main limitation. Infective endocarditis (IE) of the native pulmonary valve (PV) without predisposing factors is extremely rare. We present a case of severe pulmonary regurgitation secondary to prior native PV endocarditis, treated with two percutaneous valves implanted at the origin of the pulmonary artery branches.
Case Description
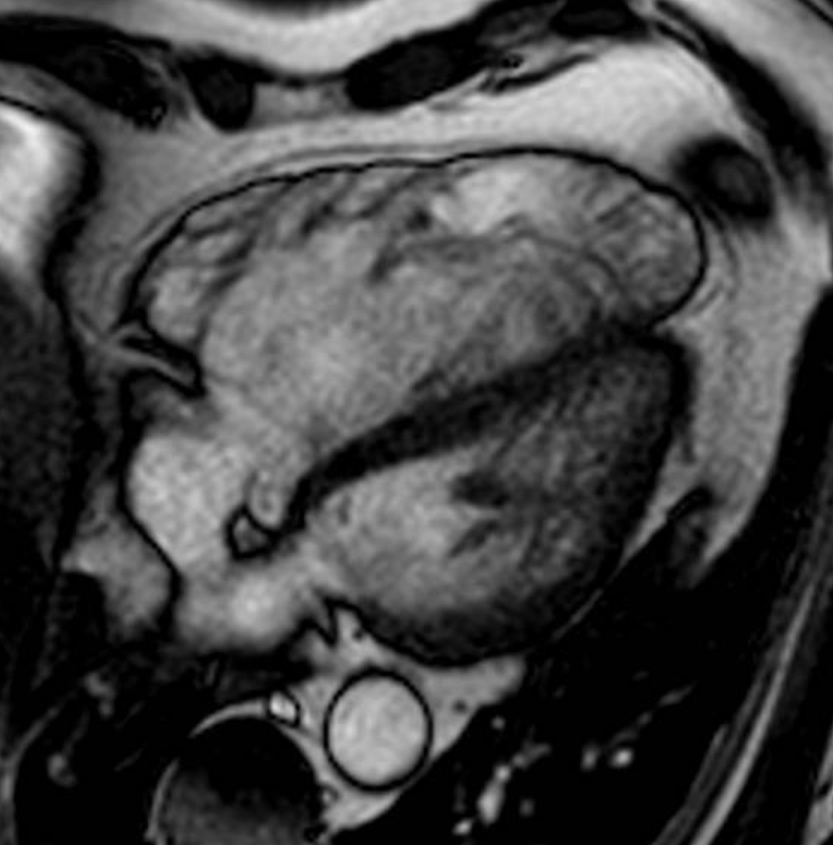
A 57-year-old male, hypertensive and former smoker, with a history of native PV IE in 2015 (no predisposing factors), treated with antibiotics and good clinical outcome, presented in May 2024 with NYHA class II dyspnea and lower limb edema. Echocardiography showed right ventricular (RV) dilation (basal: 61 mm; mid: 58 mm), TAPSE 29 mm, thickened and partially calcified PV with severe regurgitation (PHT 90 ms; diastolic reflux in branches), and no pulmonary hypertension. Cardiac MRI confirmed severe RV dilation (EDV: 387 ml; iEDV: 150 ml/m2) (Image 1), RV ejection fraction 30%, severe pulmonary regurgitation (regurgitant fraction 63%), and dilation of the pulmonary artery trunk and branches. Given symptomatic severe RV dysfunction and high surgical risk, a percutaneous approach was selected. Cardiac CT revealed a dilated RVOT (minimum diameter 35.4 x 37.7 mm; area 10.5 cm2), trunk (43.8 x 45.5 mm; area 15.1 cm2), right branch (28.6 x 29.7 mm; area 6.67 cm2), and left branch (27.6 x 30.2 mm; area 6.55 cm2). Due to unsuitable anatomy for RVOT or main trunk valve placement, two Myval N 32 valves were implanted percutaneously in each pulmonary artery branch (Image 2). The procedure was successful and uneventful. The patient improved clinically; follow-up echocardiogram showed well-functioning prostheses, minimal paravalvular regurgitation, and reduced RV dimensions (basal: 56 mm; mid: 47 mm).
Discussion
This is a rare case of severe pulmonary regurgitation due to native PV endocarditis without predisposing factors, successfully treated with bilateral percutaneous valve implantation in the pulmonary artery branches. This novel strategy offers a viable option in cases with unfavorable RVOT anatomy and emphasizes the importance of tailored interventions in complex structural heart disease.
Percutaneous treatment of pulmonary valve disease is a safe and minimally invasive alternative with favorable mid-term outcomes, especially in congenital heart disease. However, feasibility depends on right ventricular outflow tract (RVOT) anatomy, with dilation being the main limitation. Infective endocarditis (IE) of the native pulmonary valve (PV) without predisposing factors is extremely rare. We present a case of severe pulmonary regurgitation secondary to prior native PV endocarditis, treated with two percutaneous valves implanted at the origin of the pulmonary artery branches.
Case Description
A 57-year-old male, hypertensive and former smoker, with a history of native PV IE in 2015 (no predisposing factors), treated with antibiotics and good clinical outcome, presented in May 2024 with NYHA class II dyspnea and lower limb edema. Echocardiography showed right ventricular (RV) dilation (basal: 61 mm; mid: 58 mm), TAPSE 29 mm, thickened and partially calcified PV with severe regurgitation (PHT 90 ms; diastolic reflux in branches), and no pulmonary hypertension. Cardiac MRI confirmed severe RV dilation (EDV: 387 ml; iEDV: 150 ml/m2) (Image 1), RV ejection fraction 30%, severe pulmonary regurgitation (regurgitant fraction 63%), and dilation of the pulmonary artery trunk and branches. Given symptomatic severe RV dysfunction and high surgical risk, a percutaneous approach was selected. Cardiac CT revealed a dilated RVOT (minimum diameter 35.4 x 37.7 mm; area 10.5 cm2), trunk (43.8 x 45.5 mm; area 15.1 cm2), right branch (28.6 x 29.7 mm; area 6.67 cm2), and left branch (27.6 x 30.2 mm; area 6.55 cm2). Due to unsuitable anatomy for RVOT or main trunk valve placement, two Myval N 32 valves were implanted percutaneously in each pulmonary artery branch (Image 2). The procedure was successful and uneventful. The patient improved clinically; follow-up echocardiogram showed well-functioning prostheses, minimal paravalvular regurgitation, and reduced RV dimensions (basal: 56 mm; mid: 47 mm).
Discussion
This is a rare case of severe pulmonary regurgitation due to native PV endocarditis without predisposing factors, successfully treated with bilateral percutaneous valve implantation in the pulmonary artery branches. This novel strategy offers a viable option in cases with unfavorable RVOT anatomy and emphasizes the importance of tailored interventions in complex structural heart disease.
More abstracts on this topic:
4D Cardiac Magnetic Resonance Identifies Differences in Regional Strain Patterns Among Pediatric Heart Transplant Patients with Acute Rejection or Cardiac Allograft Vasculopathy
Henderson Christopher, Starnes Joseph, Samyn Margaret, Damon Bruce, Hernandez Lazaro, Goergen Craig, Soslow Jonathan, Prado Marco Aurélio, Earl Conner, Georgedurrett Kristen, Lee Simon, Nandi Deipanjan, Chan Kak-chen, Shugh Svetlana, Kikano Sandra
A Shocking Development After Peripheral Arterial InterventionAggarwal Devika, Badar Mustanser, Gowda Ramesh