Final ID: MP1341
Post-LVAD Pulsatility Index Trajectories and Their Clinical Implications: A Retrospective Study of China Multicenter LVAD Cohort
Abstract Body (Do not enter title and authors here): Introduction: Left ventricular assist devices (LVAD), widely adopted internationally, have been increasingly implemented in China as a vital life-support strategy for patients with end-stage heart failure. Non-pulsatile blood flow is a defining physiological characteristic of LVAD support. Although an association between reduced pulsatility and adverse outcomes continues to be proposed, robust clinical evidence remains lacking.
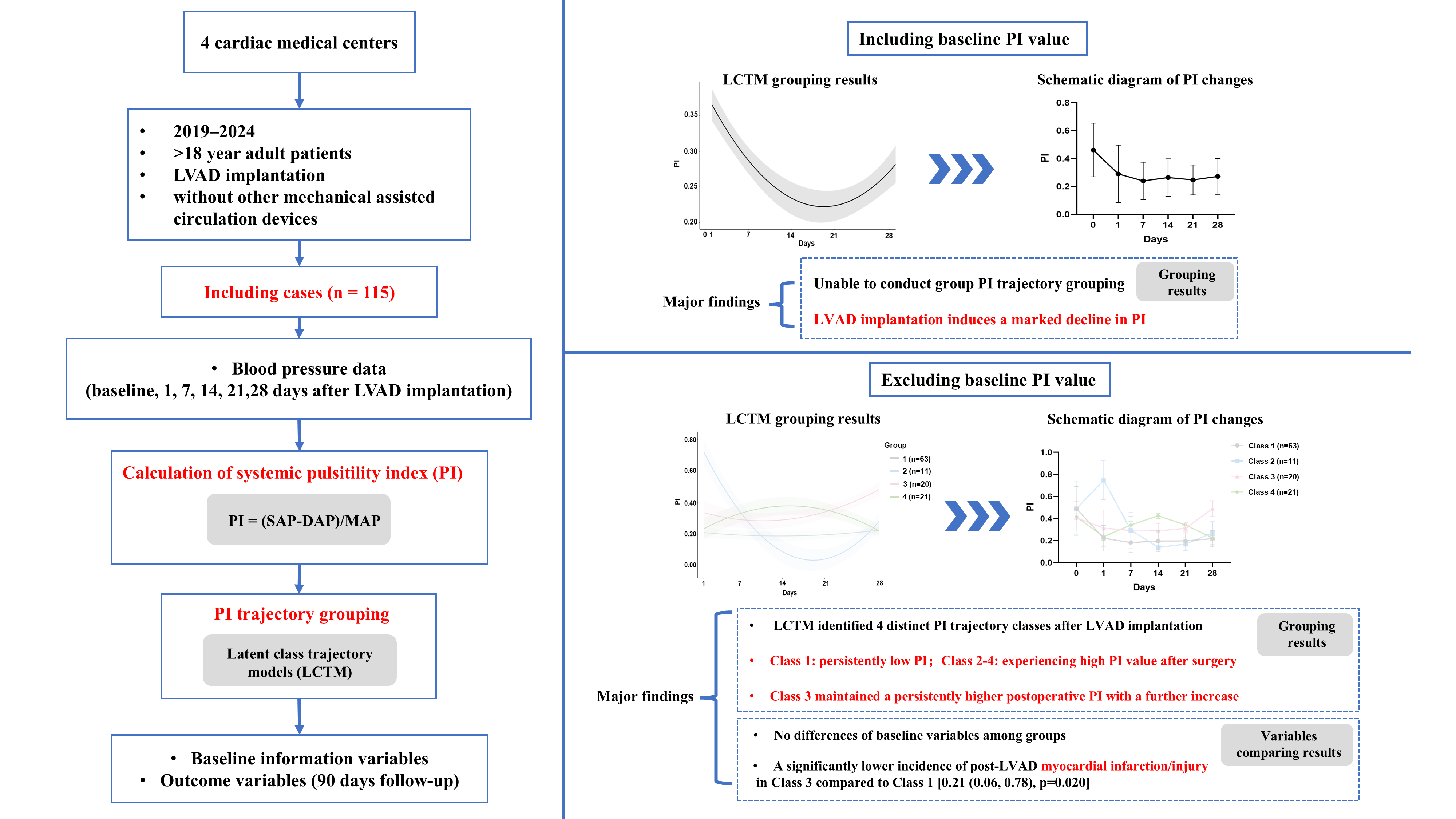
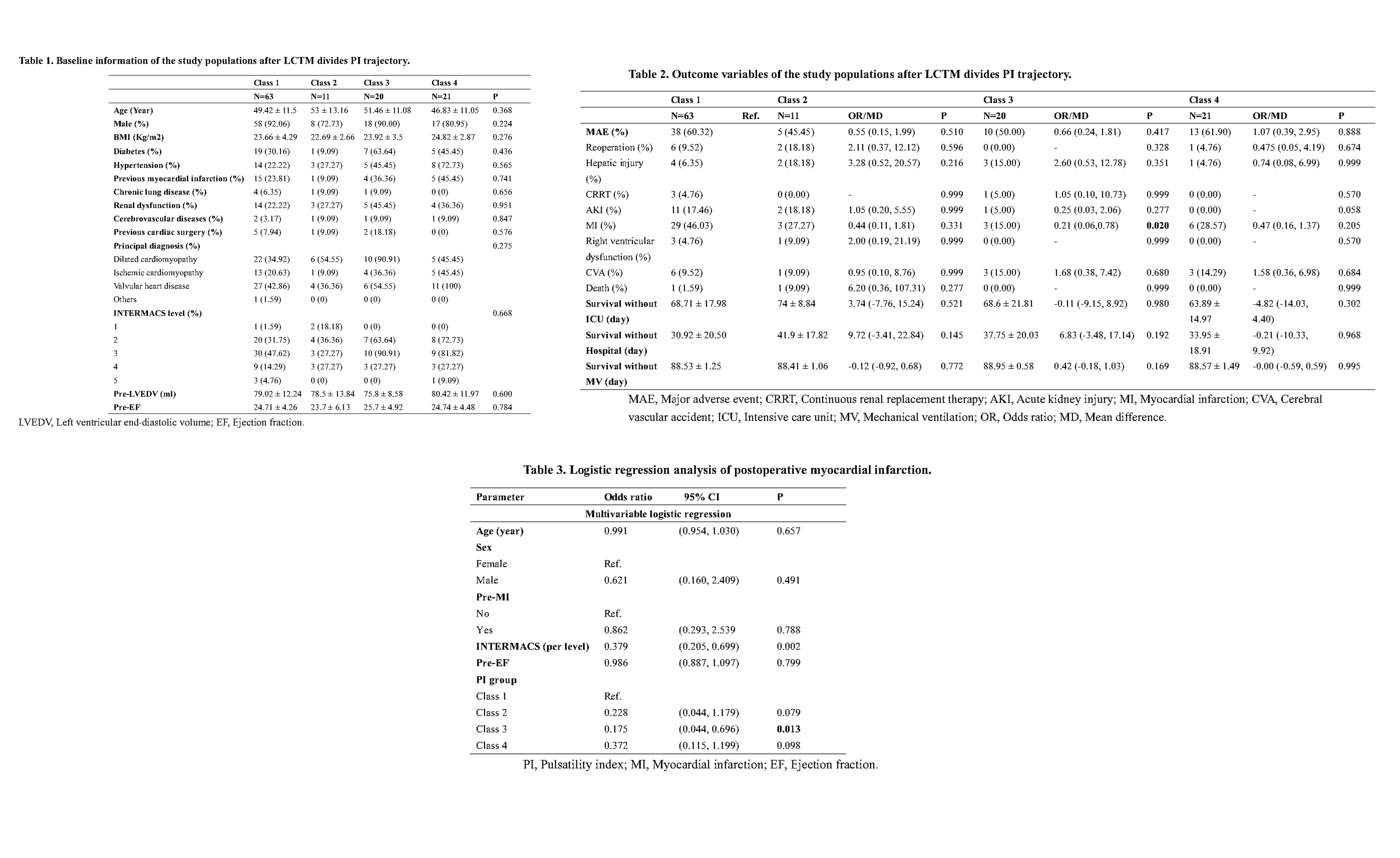
Methods: Retrospective study of adults (>18 years) receiving LVADs at four Chinese cardiac medical centers (Jan 2019 - Jul 2024) was conducted. Systemic pulsatility index (PI, calculated as pulse pressure divided by the mean arterial pressure) was derived from blood pressure measurements pre-LVAD and serially post-LVAD (days 1, 7, 14, 21, 28). Latent Class Trajectory Modeling (LCTM) identified distinct population groups based on PI trajectories; optimal model selection used lowest Bayesian Information Criterion (BIC), posterior probability >0.8, and group size >2%. The primary outcome was 90-day major adverse events (MAE: mortality or complications). Association between PI trajectories and clinical outcomes were assessed using univariable and multivariable logistic regression (adjusted for age, sex, BSA, pre-MI and INTERMACS level).
Results: Among 115 LVAD patients (mean age 49.4 years, 87.3% male, mean LVEF 24.8%), LCTM failed to identify distinct groups when including pre-LVAD PI. Overall, PI markedly declined post-implantation compared to baseline. However, LCTM using only post-LVAD data revealed four distinct PI trajectory classes. Patients with persistently higher PI post-LVAD had a significantly lower incidence of postoperative myocardial infarction/injury (MI) compared to those with persistently low PI (OR 0.21, 95% CI 0.06–0.78, p=0.020). Further logistic regression confirmed this association between post-LVAD PI trajectory and MI occurrence. No significant differences were observed in major adverse events, mortality, or other complications among trajectory groups.
Conclusion: In China's largest LVAD cohort, PI trajectory analysis revealed that patients maintaining persistently higher PI post-LVAD had a significantly lower risk of postoperative MI compared to those with persistently low PI.
Methods: Retrospective study of adults (>18 years) receiving LVADs at four Chinese cardiac medical centers (Jan 2019 - Jul 2024) was conducted. Systemic pulsatility index (PI, calculated as pulse pressure divided by the mean arterial pressure) was derived from blood pressure measurements pre-LVAD and serially post-LVAD (days 1, 7, 14, 21, 28). Latent Class Trajectory Modeling (LCTM) identified distinct population groups based on PI trajectories; optimal model selection used lowest Bayesian Information Criterion (BIC), posterior probability >0.8, and group size >2%. The primary outcome was 90-day major adverse events (MAE: mortality or complications). Association between PI trajectories and clinical outcomes were assessed using univariable and multivariable logistic regression (adjusted for age, sex, BSA, pre-MI and INTERMACS level).
Results: Among 115 LVAD patients (mean age 49.4 years, 87.3% male, mean LVEF 24.8%), LCTM failed to identify distinct groups when including pre-LVAD PI. Overall, PI markedly declined post-implantation compared to baseline. However, LCTM using only post-LVAD data revealed four distinct PI trajectory classes. Patients with persistently higher PI post-LVAD had a significantly lower incidence of postoperative myocardial infarction/injury (MI) compared to those with persistently low PI (OR 0.21, 95% CI 0.06–0.78, p=0.020). Further logistic regression confirmed this association between post-LVAD PI trajectory and MI occurrence. No significant differences were observed in major adverse events, mortality, or other complications among trajectory groups.
Conclusion: In China's largest LVAD cohort, PI trajectory analysis revealed that patients maintaining persistently higher PI post-LVAD had a significantly lower risk of postoperative MI compared to those with persistently low PI.
More abstracts on this topic:
Direct Comparison of Mechanical Circulatory Support Devices in a Porcine Model of Myocardial Infarction Complicated by Acute Mitral Regurgitation and Cardiogenic Shock
Ostadal Petr, Vondrakova Dagmar, Grus Tomas, Burkert Jan, Valerianova Anna, Neuzil Petr, Kittnar Otomar, Mlcek Mikulas
Clinical and Hemodynamic Predictors of Stabilization and Associated Complications in Patients with Cardiogenic Shock Supported with Impella 5.5Blumer Vanessa, Abraham Jacob, Li Borui, Kanwar Manreet, Garan Reshad, Sinha Shashank, Hernandez-montfort Jaime, Burkhoff Daniel, Kapur Navin