Final ID: Sa2016
Temporal Trends and Disparities in Mortality From Cardiac Arrest and Sudden Cardiac Death–Related Mortality in U.S. Adults With Diabetes: A National Population-Based Analysis
Abstract Body (Do not enter title and authors here): Introduction:
Sudden cardiac death (SCD) and cardiac arrest are major causes of mortality in individuals with diabetes, who are at increased risk due to autonomic dysfunction, accelerated atherosclerosis, and poor cardiovascular outcomes. Understanding temporal trends and subgroup disparities is critical to informing clinical and preventive strategies.
Methodology:
We analyzed U.S. multiple cause-of-death data from the CDC WONDER database (1999–2020) for adults aged ≥25 years with diabetes (ICD-10: E10–E14) and sudden cardiac arrest SCD (ICD code I46.1) or cardiac arrest, unspecified (ICD-10: I46.9). Age-adjusted mortality rates (AAMRs, per 100,000) were calculated and stratified by sex, age group, race/ethnicity, and census region. Joinpoint regression identified inflection points and annual percent changes (APCs) with 95% confidence intervals (CIs).
Results:
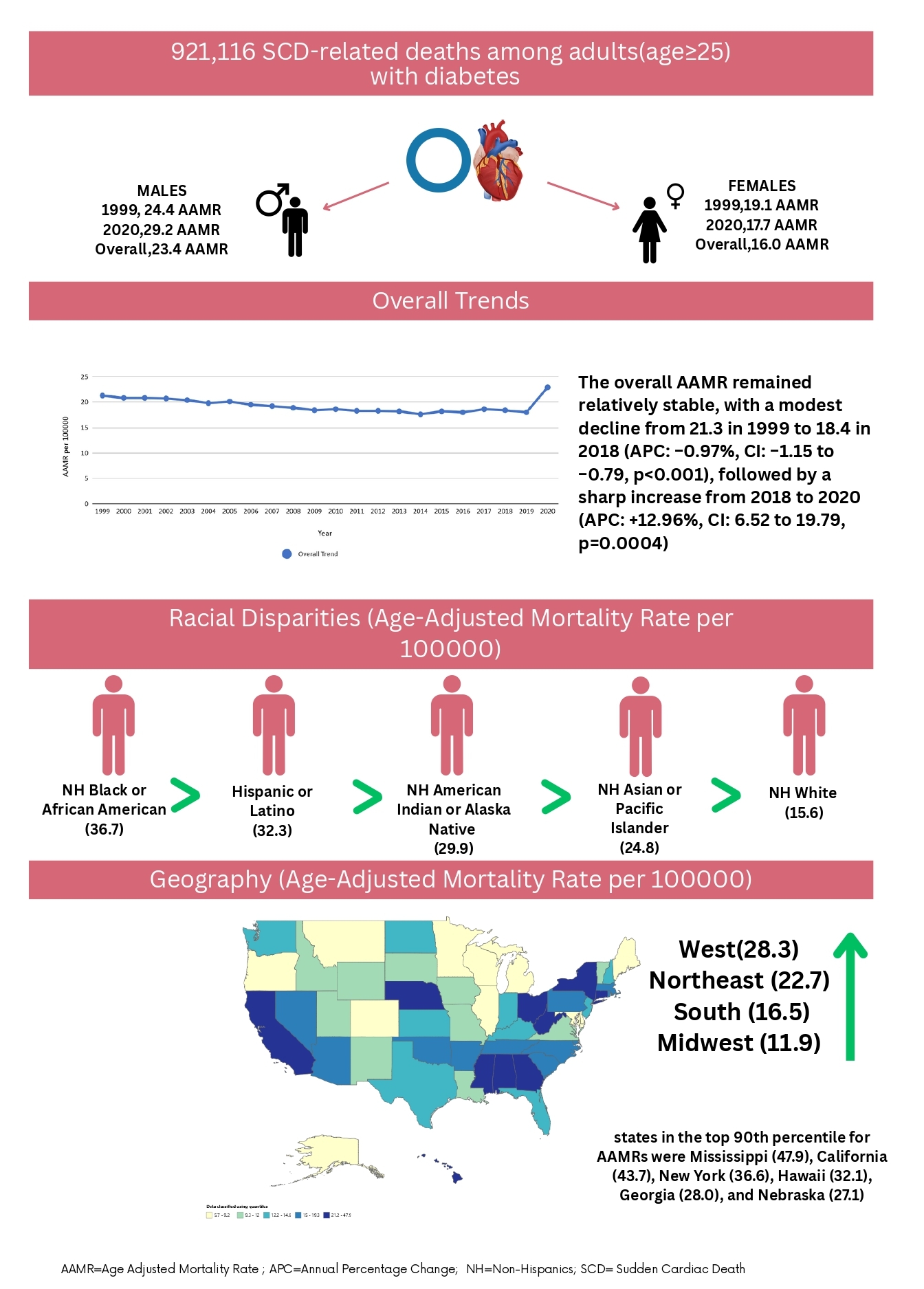
Between 1999 and 2020, there were 921,116 SCD-related deaths among adults with diabetes. The overall AAMR remained relatively stable, with a modest decline from 21.3 in 1999 to 18.4 in 2018 (APC: −0.97%, CI: −1.15 to −0.79, p<0.001), followed by a sharp increase from 2018 to 2020 (APC: +12.96%, CI: 6.52 to 19.79, p=0.0004). Males had a higher AAMR (23.4) than females (16); however, only females showed a post-2018 surge (APC +11.89% CI: 5.5 to 18.65, p=0.0009). Mortality increased with age. Adults ≥ 65 had by far the highest AAMR (71.1), followed by age 45–64 (11), and age 25–44 (1.1). Racially, AAMRs for Non-Hispanic (NH) Black were highest (36.7), followed by Hispanic or Latino (32.3), American Indian or Alaska Native (29.9), Asian or Pacific Islander (24.8) and then White (15.6). Significant post-2018 increases occurred across all racial groups except American Indian, which showed a steady rise throughout. Regionally, every U.S. census region showed a significant post-2018 inflection, with the West (28.3) and Northeast (22.7) having the highest AAMRs.
Conclusion:
Despite prior declines, SCD-related mortality among adults with diabetes has sharply increased since 2018 across nearly all demographic and geographic subgroups. These findings highlight the urgent need for targeted interventions focused on cardiovascular risk reduction, earlier detection, and addressing systemic disparities in high-risk populations.
Sudden cardiac death (SCD) and cardiac arrest are major causes of mortality in individuals with diabetes, who are at increased risk due to autonomic dysfunction, accelerated atherosclerosis, and poor cardiovascular outcomes. Understanding temporal trends and subgroup disparities is critical to informing clinical and preventive strategies.
Methodology:
We analyzed U.S. multiple cause-of-death data from the CDC WONDER database (1999–2020) for adults aged ≥25 years with diabetes (ICD-10: E10–E14) and sudden cardiac arrest SCD (ICD code I46.1) or cardiac arrest, unspecified (ICD-10: I46.9). Age-adjusted mortality rates (AAMRs, per 100,000) were calculated and stratified by sex, age group, race/ethnicity, and census region. Joinpoint regression identified inflection points and annual percent changes (APCs) with 95% confidence intervals (CIs).
Results:
Between 1999 and 2020, there were 921,116 SCD-related deaths among adults with diabetes. The overall AAMR remained relatively stable, with a modest decline from 21.3 in 1999 to 18.4 in 2018 (APC: −0.97%, CI: −1.15 to −0.79, p<0.001), followed by a sharp increase from 2018 to 2020 (APC: +12.96%, CI: 6.52 to 19.79, p=0.0004). Males had a higher AAMR (23.4) than females (16); however, only females showed a post-2018 surge (APC +11.89% CI: 5.5 to 18.65, p=0.0009). Mortality increased with age. Adults ≥ 65 had by far the highest AAMR (71.1), followed by age 45–64 (11), and age 25–44 (1.1). Racially, AAMRs for Non-Hispanic (NH) Black were highest (36.7), followed by Hispanic or Latino (32.3), American Indian or Alaska Native (29.9), Asian or Pacific Islander (24.8) and then White (15.6). Significant post-2018 increases occurred across all racial groups except American Indian, which showed a steady rise throughout. Regionally, every U.S. census region showed a significant post-2018 inflection, with the West (28.3) and Northeast (22.7) having the highest AAMRs.
Conclusion:
Despite prior declines, SCD-related mortality among adults with diabetes has sharply increased since 2018 across nearly all demographic and geographic subgroups. These findings highlight the urgent need for targeted interventions focused on cardiovascular risk reduction, earlier detection, and addressing systemic disparities in high-risk populations.
More abstracts on this topic:
Antihypertensive Medication Prescription Patterns at Baseline in the LINKED-HEARTS Program: A Comparative Analysis with American Heart Association Guidelines
Adomako Nana Ofori, Chen Yuling, Demarco Samantha, Chepkorir Joyline, Owusu Nti Kezia, Slone Sarah, Commodore-mensah Yvonne, Himmelfarb Cheryl
A Body Shape Index at Age 25-64 Predicts Mortality and CHD HospitalizationShafran Itamar, Krakauer Nir, Krakauer Jesse, Cohen Gali, Gerber Yariv