Final ID: MP2313
Forecasting Mortality Associated with Obstructive Sleep Apnea and Sudden Cardiac Death Among Older Adults in the U.S. (1999–2035) Using Machine Learning Models.
Abstract Body (Do not enter title and authors here): Background: Obstructive sleep apnea (OSA) is an established trigger for sudden cardiac death (SCD), yet national mortality patterns and forward-looking risk remain incompletely defined.
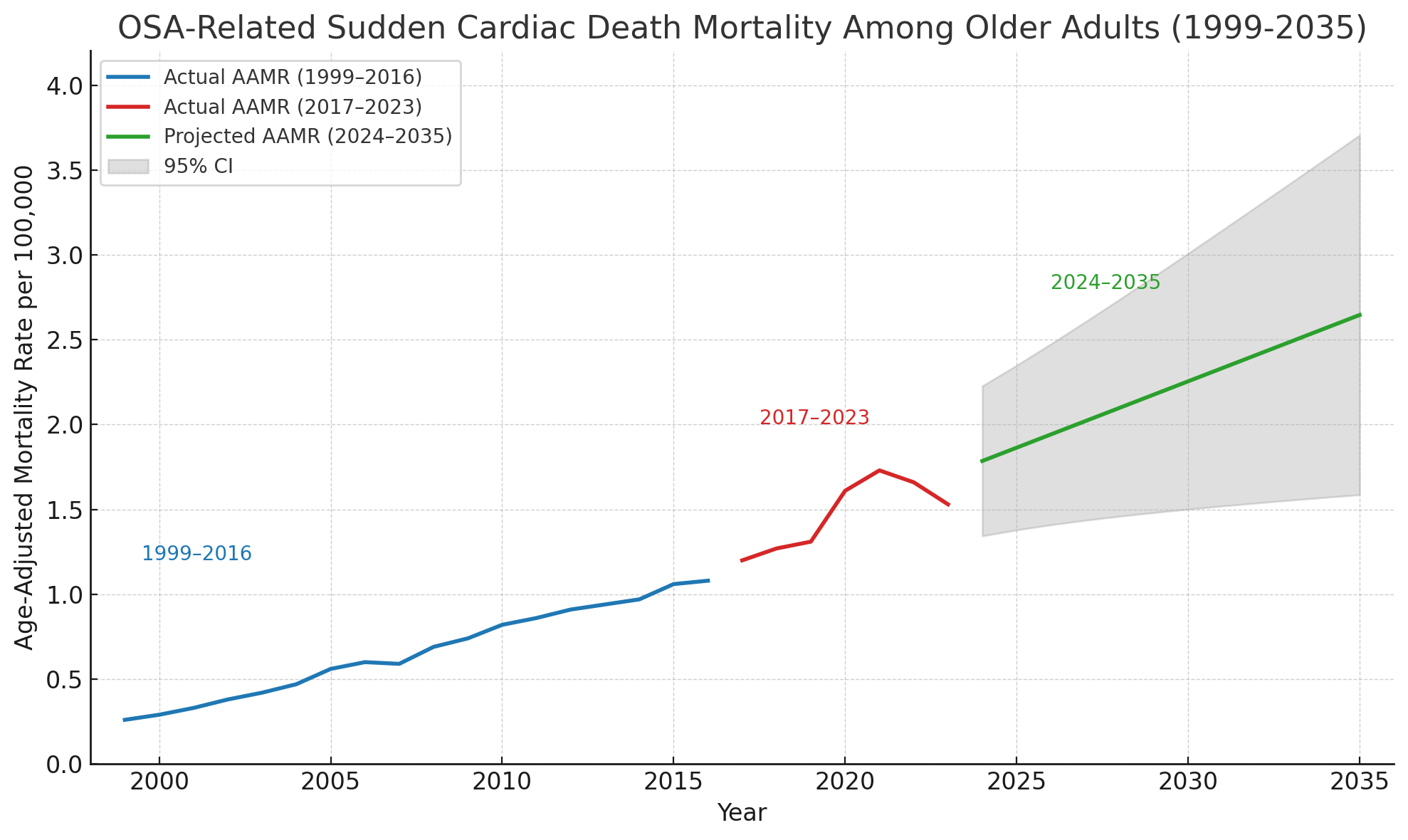
Methodology: U.S. death data (1999–2023) were obtained from CDC WONDER, including co-listed ICD-10 codes G47.3 (obstructive sleep apnea) and I46 (cardiac arrest). Age-adjusted mortality rates (AAMRs) per million were standardized to the 2000 U.S. census. Temporal trends were assessed using Joinpoint regression to calculate average annual percent change (AAPC). Forecasting was performed using a stacked long short-term memory (LSTM) model, validated against ARIMA baselines. Bootstrapped 95% prediction intervals were derived from 1,000 resamples.
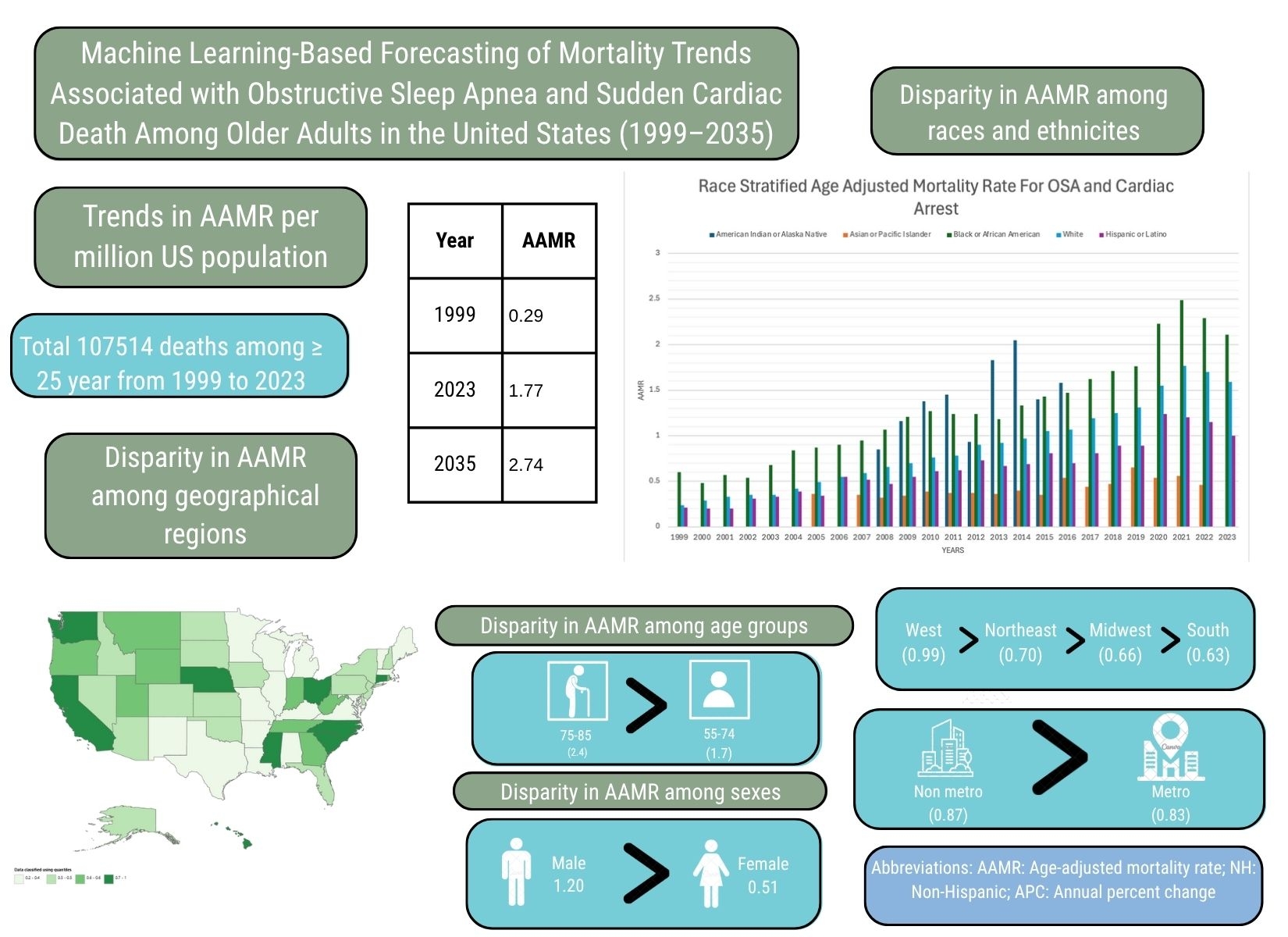
Results: From 1999 to 2023, 53,105 U.S. deaths involved both obstructive sleep apnea and cardiac arrest. The national age-adjusted mortality rate (AAMR) rose sixfold from 0.29 to 1.77 per 100,000 (AAPC: 7.21%; 95% CI: 6.61–8.04; P < 0.000001). All adult age groups saw rising mortality, with the steepest increases in those aged 85+ (AAPC: 11.60%) and 75–84 (AAPC: 8.71%). Rates also rose significantly in younger groups (35–74), with AAPCs ranging from 5.38% to 7.34%. Males peaked at an AAMR of 2.49 in 2021, dropping to 2.17 by 2023, while females plateaued at ~1.05 after 2021. White individuals had the highest burden (AAPC: 8.00%), followed by Black Americans (AAPC: 6.26%). Non-metropolitan counties exceeded metro areas in 2020 (1.76 vs. 1.57 per 100,000), with both showing strong growth (AAPCs: 8.45% and 8.67%).
All U.S. regions saw sharp increases during the COVID-19 era. A long short-term memory (LSTM) neural network, validated against ARIMA, projects AAMRs to reach 2.74 by 2033 (projected APC ≈ 4.3%), aligning with ARIMA's AAPC of 4.33% for 2024–2035. The highest mortality rates occurred in Mississippi, Alabama, and Oklahoma, up to four times greater than in the lowest-burden states like Hawaii, Massachusetts, and California.
Conclusion: OSA-related SCD mortality has risen markedly since 1999, with disproportionate burdens in men, Black Americans, and rural residents. Machine-learning projections indicate continued escalation over the next decade despite the recent plateau, highlighting an urgent need for earlier detection and treatment of OSA.
Methodology: U.S. death data (1999–2023) were obtained from CDC WONDER, including co-listed ICD-10 codes G47.3 (obstructive sleep apnea) and I46 (cardiac arrest). Age-adjusted mortality rates (AAMRs) per million were standardized to the 2000 U.S. census. Temporal trends were assessed using Joinpoint regression to calculate average annual percent change (AAPC). Forecasting was performed using a stacked long short-term memory (LSTM) model, validated against ARIMA baselines. Bootstrapped 95% prediction intervals were derived from 1,000 resamples.
Results: From 1999 to 2023, 53,105 U.S. deaths involved both obstructive sleep apnea and cardiac arrest. The national age-adjusted mortality rate (AAMR) rose sixfold from 0.29 to 1.77 per 100,000 (AAPC: 7.21%; 95% CI: 6.61–8.04; P < 0.000001). All adult age groups saw rising mortality, with the steepest increases in those aged 85+ (AAPC: 11.60%) and 75–84 (AAPC: 8.71%). Rates also rose significantly in younger groups (35–74), with AAPCs ranging from 5.38% to 7.34%. Males peaked at an AAMR of 2.49 in 2021, dropping to 2.17 by 2023, while females plateaued at ~1.05 after 2021. White individuals had the highest burden (AAPC: 8.00%), followed by Black Americans (AAPC: 6.26%). Non-metropolitan counties exceeded metro areas in 2020 (1.76 vs. 1.57 per 100,000), with both showing strong growth (AAPCs: 8.45% and 8.67%).
All U.S. regions saw sharp increases during the COVID-19 era. A long short-term memory (LSTM) neural network, validated against ARIMA, projects AAMRs to reach 2.74 by 2033 (projected APC ≈ 4.3%), aligning with ARIMA's AAPC of 4.33% for 2024–2035. The highest mortality rates occurred in Mississippi, Alabama, and Oklahoma, up to four times greater than in the lowest-burden states like Hawaii, Massachusetts, and California.
Conclusion: OSA-related SCD mortality has risen markedly since 1999, with disproportionate burdens in men, Black Americans, and rural residents. Machine-learning projections indicate continued escalation over the next decade despite the recent plateau, highlighting an urgent need for earlier detection and treatment of OSA.
More abstracts on this topic:
Carotid body ablation reduces hypertension following long-term intermittent hypoxia by regulating brainstem glial cell activation
Iturriaga Rodrigo, Pereyra Katherine, Vicencio Sinay, Bernal Ignacio, Diaz-jara Esteban, Del Rio Rodrigo
Evaluating a Single-Lead, Mobile Electrocardiogram for Screening of Atrial Fibrillation in Patients with Obstructive Sleep ApneaMittal Ajay, Savu Victor, Patel Mansi, Kapadia Kevin, Segal Mark