Final ID: MP2089
Sludgy Cors: Phlebotomy for Testosterone-Induced Polycythemia in Acute Coronary Syndrome
Abstract Body (Do not enter title and authors here): Description of Case
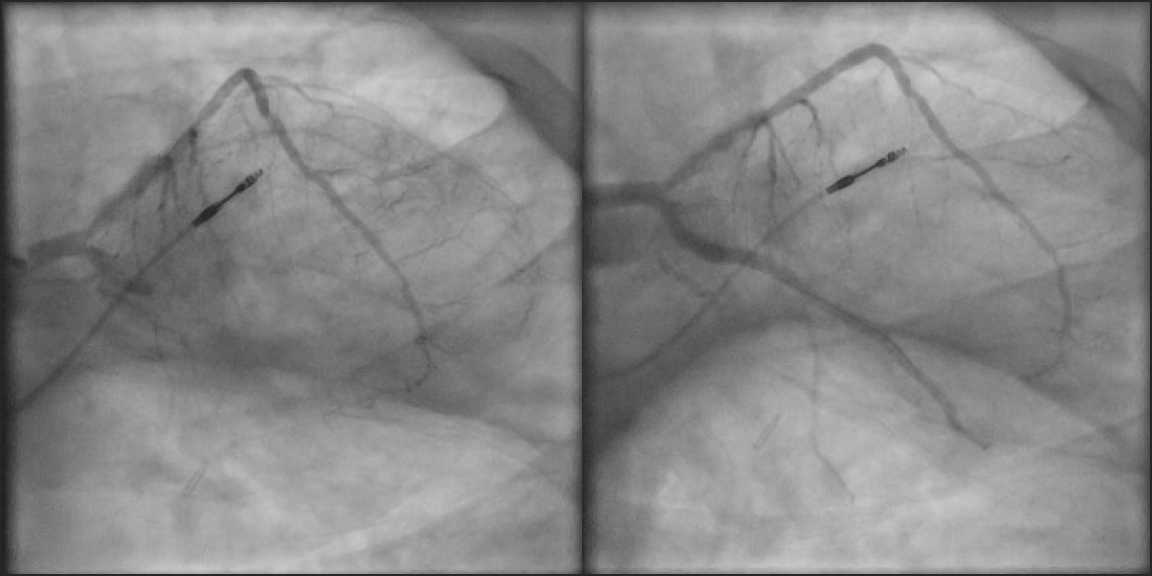
A 58-year-old male with history of primary hypogonadism on testosterone replacement therapy, coronary artery disease with prior myocardial infarction, type 2 diabetes, hypertension, hyperlipidemia, obesity, and obstructive sleep apnea on home CPAP presented with typical anginal chest pain. EKG was consistent with inferior STEMI. He was taken for emergent coronary angiography, revealing the culprit lesion: 100% occlusion of the left circumflex coronary artery (LCx) with TIMI 1 flow. Percutaneous Coronary Intervention (PCI) was performed with placement of two drug-eluting stents, and he was given loading doses of dual antiplatelet therapy. There was significant thrombus present requiring manual aspiration thrombectomy, with intravascular ultrasound confirming underlying atherosclerosis. Ultimately, TIMI 3 flow was achieved. Post-PCI, the patient had significant anginal chest pain refractory to medical management. EKG demonstrated resolution of ST elevations, and echocardiogram showed moderately reduced ejection fraction without pericardial effusion or structural complications. His initial hemoglobin was 23.1 (hematocrit 65%), and testosterone levels were markedly elevated above 1,500.
We suspected coronary thrombosis may have been partially driven by hyper viscosity from polycythemia, so we performed three therapeutic phlebotomy treatments of 500mL each and gave three one-liter intravenous fluid boluses, until hemoglobin levels were below 18. His chest pain improved markedly after phlebotomy, and he was discharged with close cardiology and endocrinology follow-up. JAK2 mutation test was negative, and testosterone supplementation was discontinued for the interim.
Discussion
Only observational data exists thus far, but testosterone-induced polycythemia has been noted as a risk factor for major adverse cardiac events (MACE) in men on testosterone therapy with hematocrit>52% compared to those on therapy with hematocrit<52%1. Moreover, any degree of polycythemia is associated with increased MACE as early as 3 months after testosterone initiation2. Phlebotomy is mainstay treatment for JAK2-positive polycythemia, targeting hematocrit<45% to reduce MACE3. This case demonstrates how ACS in the setting of polycythemia may present with a thrombotic phenotype in younger patients. Furthermore, post-PCI chest pain may be alleviated with therapeutic phlebotomy when hematocrit is dangerously high, regardless of JAK2 positivity.
A 58-year-old male with history of primary hypogonadism on testosterone replacement therapy, coronary artery disease with prior myocardial infarction, type 2 diabetes, hypertension, hyperlipidemia, obesity, and obstructive sleep apnea on home CPAP presented with typical anginal chest pain. EKG was consistent with inferior STEMI. He was taken for emergent coronary angiography, revealing the culprit lesion: 100% occlusion of the left circumflex coronary artery (LCx) with TIMI 1 flow. Percutaneous Coronary Intervention (PCI) was performed with placement of two drug-eluting stents, and he was given loading doses of dual antiplatelet therapy. There was significant thrombus present requiring manual aspiration thrombectomy, with intravascular ultrasound confirming underlying atherosclerosis. Ultimately, TIMI 3 flow was achieved. Post-PCI, the patient had significant anginal chest pain refractory to medical management. EKG demonstrated resolution of ST elevations, and echocardiogram showed moderately reduced ejection fraction without pericardial effusion or structural complications. His initial hemoglobin was 23.1 (hematocrit 65%), and testosterone levels were markedly elevated above 1,500.
We suspected coronary thrombosis may have been partially driven by hyper viscosity from polycythemia, so we performed three therapeutic phlebotomy treatments of 500mL each and gave three one-liter intravenous fluid boluses, until hemoglobin levels were below 18. His chest pain improved markedly after phlebotomy, and he was discharged with close cardiology and endocrinology follow-up. JAK2 mutation test was negative, and testosterone supplementation was discontinued for the interim.
Discussion
Only observational data exists thus far, but testosterone-induced polycythemia has been noted as a risk factor for major adverse cardiac events (MACE) in men on testosterone therapy with hematocrit>52% compared to those on therapy with hematocrit<52%1. Moreover, any degree of polycythemia is associated with increased MACE as early as 3 months after testosterone initiation2. Phlebotomy is mainstay treatment for JAK2-positive polycythemia, targeting hematocrit<45% to reduce MACE3. This case demonstrates how ACS in the setting of polycythemia may present with a thrombotic phenotype in younger patients. Furthermore, post-PCI chest pain may be alleviated with therapeutic phlebotomy when hematocrit is dangerously high, regardless of JAK2 positivity.
More abstracts on this topic:
Artificial Intelligence for Predicting Primary Antegrade Wiring Success of Chronic Total Occlusion Crossing
Alexandrou Michaella, Alaswad Khaldoon, Basir Mir, Davies Rhian, Jaffer Farouc, Nicholson William, Azzalini Lorenzo, Gorgulu Sevket, Khatri Jaikirshan, Bangalore Sripal, Rangan Bavana, Rempakos Athanasios, Mastrodemos Olga, Burke M Nicholas, Sandoval Yader, Brilakis Emmanouil, Mutlu Deniz, Strepkos Dimitrios, Carvalho Pedro, Al-ogaili Ahmed, Bahbah Ali, Anastasios Milkas, Tsiafoutis Ioannis
Cardiac Arrhythmia-Related Mortality in Adults with Aplastic Anemia in the United States: A 25-Year Nationwide Analysis (1999–2023)Ahmad Husnain, Patel Palak, Ali Muhammad Faizan, Oza Jaykumar, Rahim Muhammad