Final ID: Sa1029
Hypoxemia Beyond the Heart: A Case of Hepatopulmonary Syndrome Masquerading as Cardiac Dyspnea
Abstract Body (Do not enter title and authors here): Hepatopulmonary syndrome (HPS), a serious yet underrecognized cause of hypoxia in patients with liver disease, can mimic cardiopulmonary pathology. Multimodal cardiac imaging plays a critical role in distinguishing HPS from intracardiac shunts. Median survival is 10.6 months if untreated, making timely diagnosis essential.
Case:
A 55-year-old Peruvian female with cirrhosis from metabolic dysfunction-associated steatotic liver disease, type 2 diabetes mellitus and hypertension presented with worsening shortness of breath and increasing oxygen requirements from her baseline (3 L/min via nasal cannula). She was hypotensive and hypoxic, requiring high-flow nasal cannula. Physical examination revealed bilateral decreased breath sounds and digital clubbing. Laboratory findings were notable for normocytic anemia, mild thrombocytopenia, elevated transaminases, procalcitonin, and lactate. Chest computed tomography (CT) suggested pulmonary edema and signs of portal hypertension with varices.
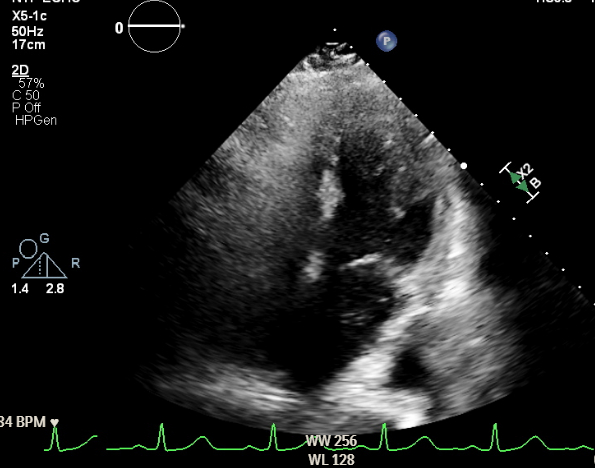
An outpatient transthoracic echocardiogram (TTE) with bubble study had shown early microbubbles in the left atrium, raising concern for an intracardiac shunt. Transesophageal echocardiography (TEE) was deferred due to esophageal varices. Repeat inpatient contrast TTE revealed a moderately dilated left ventricle but no evidence of ASD or PFO. Cardiac Magnetic resonance imaging (MRI) demonstrated a normal Qp:Qs and no anomalous venous return or intracardiac shunt. Due to persistent hypoxemia, the patient was transferred to a tertiary center. There, repeat contrast TTE showed innumerable microbubbles in the left heart after four cardiac cycles suggestive of an intrapulmonary shunt. Chest CT with contrast showed no structural evidence of an intrapulmonary shunt. Right heart catheterization confirmed a right-to-left shunt with Qp:Qs = 0.6, and microbubbles were visualized crossing from the pulmonary artery into the left atrium on intracardiac echocardiography (ICE),
Discussion:
This case demonstrates the crucial role of multimodality cardiac imaging—including contrast echo, MRI, RHC, and ICE—in identifying HPS in a cirrhotic patient with unexplained hypoxemia. In cardiology clinics, such patients may be misdiagnosed with intracardiac shunts or heart failure, delaying a life-limiting diagnosis. Early recognition of HPS can significantly impact outcomes by prompting timely transplant referral.
Case:
A 55-year-old Peruvian female with cirrhosis from metabolic dysfunction-associated steatotic liver disease, type 2 diabetes mellitus and hypertension presented with worsening shortness of breath and increasing oxygen requirements from her baseline (3 L/min via nasal cannula). She was hypotensive and hypoxic, requiring high-flow nasal cannula. Physical examination revealed bilateral decreased breath sounds and digital clubbing. Laboratory findings were notable for normocytic anemia, mild thrombocytopenia, elevated transaminases, procalcitonin, and lactate. Chest computed tomography (CT) suggested pulmonary edema and signs of portal hypertension with varices.
An outpatient transthoracic echocardiogram (TTE) with bubble study had shown early microbubbles in the left atrium, raising concern for an intracardiac shunt. Transesophageal echocardiography (TEE) was deferred due to esophageal varices. Repeat inpatient contrast TTE revealed a moderately dilated left ventricle but no evidence of ASD or PFO. Cardiac Magnetic resonance imaging (MRI) demonstrated a normal Qp:Qs and no anomalous venous return or intracardiac shunt. Due to persistent hypoxemia, the patient was transferred to a tertiary center. There, repeat contrast TTE showed innumerable microbubbles in the left heart after four cardiac cycles suggestive of an intrapulmonary shunt. Chest CT with contrast showed no structural evidence of an intrapulmonary shunt. Right heart catheterization confirmed a right-to-left shunt with Qp:Qs = 0.6, and microbubbles were visualized crossing from the pulmonary artery into the left atrium on intracardiac echocardiography (ICE),
Discussion:
This case demonstrates the crucial role of multimodality cardiac imaging—including contrast echo, MRI, RHC, and ICE—in identifying HPS in a cirrhotic patient with unexplained hypoxemia. In cardiology clinics, such patients may be misdiagnosed with intracardiac shunts or heart failure, delaying a life-limiting diagnosis. Early recognition of HPS can significantly impact outcomes by prompting timely transplant referral.
More abstracts on this topic:
Chronic cerebral hypoperfusion impairs brain iron metabolism in aged mice
Monga Sheelu, Moruno-manchon Jose
Implementation of a Standard Hydration Protocol Improves Compliance of Pre-procedural Hydration, Reducing the Incidence of Contrast-Induced Acute Kidney Injury (CI-AKI) After Percutaneous Coronary Intervention (PCI)Lee Ju Hyun, Avendano Amilcar, Nutt Rebecca