Final ID: MP187
Short Term Heart Failure Readmission Risk Prediction from Single Lead ECG-AI Driven BNP Estimation
Abstract Body (Do not enter title and authors here): Background: Heart failure (HF) accounts for the highest hospital readmission rates in the United States, with its annual direct medical costs projected to exceed $50 billion by 2030. There is a lack of noninvasive, low cost, remotely-applicable, and scalable tools for early identification of HF decompensation leading to readmission.
Hypothesis: We hypothesized that lead I ECG-AI-based estimates of BNP derived from HF admission and discharge ECGs could independently predict short-term risk for HF readmission.
Methods: A multi-task convolutional neural network using only lead I ECG waveforms was developed to estimate lab-based BNP values and clinical strata (low: <100 pg/mL, elevated: >500 pg/mL) using EHR data from Atrium Health Wake Forest Baptist (WF) (102,311 ECG-BNP pairs from 54,526 patients). This model was then applied, without fine-tuning, to admission and discharge ECGs in an independent cohort of patients hospitalized for HF at WF (n=793) to determine the association between changes in AI-predicted elevated BNP and short-term readmission using logistic regression (LR) with and without adjustment for age, sex, race. HF readmission prediction performance for days 2-5 post discharge was evaluated using AUCs.
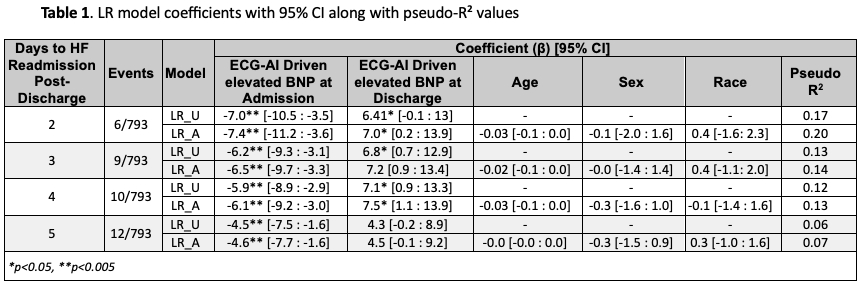
Results: The multi-task lead I ECG-AI model achieved AUCs of 0.83 (95% CI: 0.83–0.84) and 0.83 (95% CI: 0.82–0.84) for identifying low (<100 pg/mL) and high (>500 pg/mL) BNP levels, respectively. The Spearman correlation between actual and predicted BNP values on the WF holdout set (n=10,264) was ρ = 0.69, p < 0.01. Relative changes in AI-predicted elevated BNP were associated with HF readmission, with AUCs of 0.77 (days 2–4) and 0.69 (day 5). When building outcome-informed LR model based on AI-predicted elevated BNP values at admission and discharge, we achieved AUCs of 0.80 (day 2), 0.77 (days 3–4), and 0.69 (day 5). After adjustment for demographics (LR_A), we obtained AUCs of 0.88 (day 2), 0.83 (day 3), 0.82 (day 4), and 0.70 (day 5), all p < 0.05. Model coefficients are shown in Table 1.
Conclusion: Analysis of admission and discharge lead I ECGs via AI can predict short-term readmission risk with high accuracy. Since lead I ECGs are easily obtained from smart watch technology, these findings lay the groundwork for potential use of lead I ECGs for remote outpatient surveillance post-discharge to assess risk of readmission.
Hypothesis: We hypothesized that lead I ECG-AI-based estimates of BNP derived from HF admission and discharge ECGs could independently predict short-term risk for HF readmission.
Methods: A multi-task convolutional neural network using only lead I ECG waveforms was developed to estimate lab-based BNP values and clinical strata (low: <100 pg/mL, elevated: >500 pg/mL) using EHR data from Atrium Health Wake Forest Baptist (WF) (102,311 ECG-BNP pairs from 54,526 patients). This model was then applied, without fine-tuning, to admission and discharge ECGs in an independent cohort of patients hospitalized for HF at WF (n=793) to determine the association between changes in AI-predicted elevated BNP and short-term readmission using logistic regression (LR) with and without adjustment for age, sex, race. HF readmission prediction performance for days 2-5 post discharge was evaluated using AUCs.
Results: The multi-task lead I ECG-AI model achieved AUCs of 0.83 (95% CI: 0.83–0.84) and 0.83 (95% CI: 0.82–0.84) for identifying low (<100 pg/mL) and high (>500 pg/mL) BNP levels, respectively. The Spearman correlation between actual and predicted BNP values on the WF holdout set (n=10,264) was ρ = 0.69, p < 0.01. Relative changes in AI-predicted elevated BNP were associated with HF readmission, with AUCs of 0.77 (days 2–4) and 0.69 (day 5). When building outcome-informed LR model based on AI-predicted elevated BNP values at admission and discharge, we achieved AUCs of 0.80 (day 2), 0.77 (days 3–4), and 0.69 (day 5). After adjustment for demographics (LR_A), we obtained AUCs of 0.88 (day 2), 0.83 (day 3), 0.82 (day 4), and 0.70 (day 5), all p < 0.05. Model coefficients are shown in Table 1.
Conclusion: Analysis of admission and discharge lead I ECGs via AI can predict short-term readmission risk with high accuracy. Since lead I ECGs are easily obtained from smart watch technology, these findings lay the groundwork for potential use of lead I ECGs for remote outpatient surveillance post-discharge to assess risk of readmission.
More abstracts on this topic:
Advancing Age, ASA Class, Sex, Functional Status, and Comorbidities as Predictors of Perioperative Cardiac Arrest Following Total Hip Arthroplasty: A National Cohort Study
Hussain Abdur-rehman, Soni Ashesh, Stead Thor, Persaud Nadiya, Ganti Latha
A novel XAI framework for explainable AI-ECG using generative counterfactual-based XAILee Min Sung, Jang Jong-hwan, Jo Yong-yeon, Kang Sora, Son Jeong Min, Lee Hak Seung, Kwon Joon-myoung