Final ID: MP2287
Reevaluating Lipoprotein(a) Levels and Risk of All-Cause Mortality in the Setting of Primary Prevention: A Retrospective Cohort Study
Abstract Body (Do not enter title and authors here): Introduction: Elevated lipoprotein(a) [Lp(a)] levels (≥30 mg/dL or ≥50 mg/dL) have been associated with increased risk of cardiovascular diseases (CVD), including myocardial infarction and aortic stenosis. However, its association with all-cause mortality (ACM) in the setting of primary prevention remains unclear, with conflicting evidence regarding the cutoff associated with increased mortality risk.
Objective: To assess the association between elevated Lp(a) and risk of ACM in the context of primary prevention.
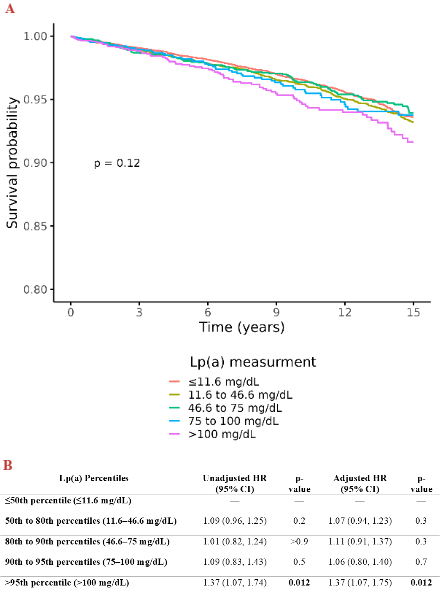
Methods: In this retrospective cohort study, we included adult patients (≥18 years old) who had at least one measurement of Lp(a) at any of the three Mayo Clinic sites between 2007 and 2024, with no history of CVDs (i.e., coronary artery disease, ischemic stroke/transient ischemic attack, or peripheral arterial disease) at the time of Lp(a) measurement. Lp(a) levels were categorized based on the following percentiles: ≤50th percentile (≤11.6 mg/dL), 50th to 80th percentiles (11.6–46.6 mg/dL), 80th to 90th percentiles (46.6–75 mg/dL), 90th to 95th percentiles (75–100 mg/dL), and >95th percentile (>100 mg/dL). Survival probabilities up to 15 years were compared across Lp(a) percentile categories using the Kaplan–Meier estimator and log-rank test. Additionally, univariable and multivariable Cox regression analyses were conducted to adjust for potential CV confounders and to quantify this association.
Results: A total of 42,770 patients (median age: 53 years and 54% males) were included. We found no significant difference in survival probabilities between the Lp(a) categories based on the overall log-rank test (p=0.12; Figure 1A). In the univariable analysis, only patients with Lp(a) >95th percentile (>100 mg/dL) had a statistically significant higher risk of ACM [hazard ratio (HR): 1.37; 95%CI: 1.07–1.74; p=0.012], compared to patients with Lp(a) <50th percentile (<11.6 mg/dL). Similarly, after adjusting for potential CV risk factors, only those with Lp(a) >95th percentile (>100 mg/dL) showed a significantly higher risk of ACM (adjusted HR: 1.37; 95%CI: 1.07–1.75; p=0.012, Figure 1B).
Conclusion: In the setting of primary prevention, only very high Lp(a) levels (≥100 mg/dL) were independently associated with increased risk of ACM, suggesting that higher Lp(a) thresholds may be more relevant for identifying individuals at increased risk of ACM than the conventional ≥50 mg/dL cutoff.
Objective: To assess the association between elevated Lp(a) and risk of ACM in the context of primary prevention.
Methods: In this retrospective cohort study, we included adult patients (≥18 years old) who had at least one measurement of Lp(a) at any of the three Mayo Clinic sites between 2007 and 2024, with no history of CVDs (i.e., coronary artery disease, ischemic stroke/transient ischemic attack, or peripheral arterial disease) at the time of Lp(a) measurement. Lp(a) levels were categorized based on the following percentiles: ≤50th percentile (≤11.6 mg/dL), 50th to 80th percentiles (11.6–46.6 mg/dL), 80th to 90th percentiles (46.6–75 mg/dL), 90th to 95th percentiles (75–100 mg/dL), and >95th percentile (>100 mg/dL). Survival probabilities up to 15 years were compared across Lp(a) percentile categories using the Kaplan–Meier estimator and log-rank test. Additionally, univariable and multivariable Cox regression analyses were conducted to adjust for potential CV confounders and to quantify this association.
Results: A total of 42,770 patients (median age: 53 years and 54% males) were included. We found no significant difference in survival probabilities between the Lp(a) categories based on the overall log-rank test (p=0.12; Figure 1A). In the univariable analysis, only patients with Lp(a) >95th percentile (>100 mg/dL) had a statistically significant higher risk of ACM [hazard ratio (HR): 1.37; 95%CI: 1.07–1.74; p=0.012], compared to patients with Lp(a) <50th percentile (<11.6 mg/dL). Similarly, after adjusting for potential CV risk factors, only those with Lp(a) >95th percentile (>100 mg/dL) showed a significantly higher risk of ACM (adjusted HR: 1.37; 95%CI: 1.07–1.75; p=0.012, Figure 1B).
Conclusion: In the setting of primary prevention, only very high Lp(a) levels (≥100 mg/dL) were independently associated with increased risk of ACM, suggesting that higher Lp(a) thresholds may be more relevant for identifying individuals at increased risk of ACM than the conventional ≥50 mg/dL cutoff.
More abstracts on this topic:
Apolipoprotein A1 infusion in patients with Acute Myocardial Infarction: A Systematic Review and Meta-analysis of randomized trials
Prata Alonzo, Gioli-pereira Luciana, Fukunaga Christian, Katsuyama Eric, Coan Ana Carolina, Scardini Pedro Gabriel, Petri Santos Pinheiro Rafael, Falco Neto Wilson, Fernandes Julia, Andrade Naieli
Association Between Elevated Lipoprotein(a) and New-Onset Atrial Fibrillation: A Retrospective Analysis Using the TriNetX Research NetworkQadeer Abdul, Akbar Usman, Ahmed Faizan, Shabbir Muhammad Raffey, Aamir Muhammad, Fouad Michele, Khan Allahdad, Khawar Muneeb, Pathak Prutha, Hassan Furqan, Hotwani Priya, Khan Sardar Muhammad Imran, Shafique Nouman