Final ID: MP2294
Lipoprotein(a) and Metabolic Syndrome are Associated with Increased Risk of Coronary Heart Disease
Abstract Body (Do not enter title and authors here): Background
Lipoprotein(a) [Lp(a)] and metabolic syndrome (MetS) are well-established risk factors for cardiovascular disease. Recent evidence suggests that high Lp(a) levels may increase the risk of coronary heart disease (CHD) in patients with diabetes, raising the question of whether similar interactions exist between Lp(a) and metabolic syndrome. We aimed to evaluate the joint association of Lp(a) and MetS with incident CHD risk in a large, multi-ethnic, prospective cohort.
Methods
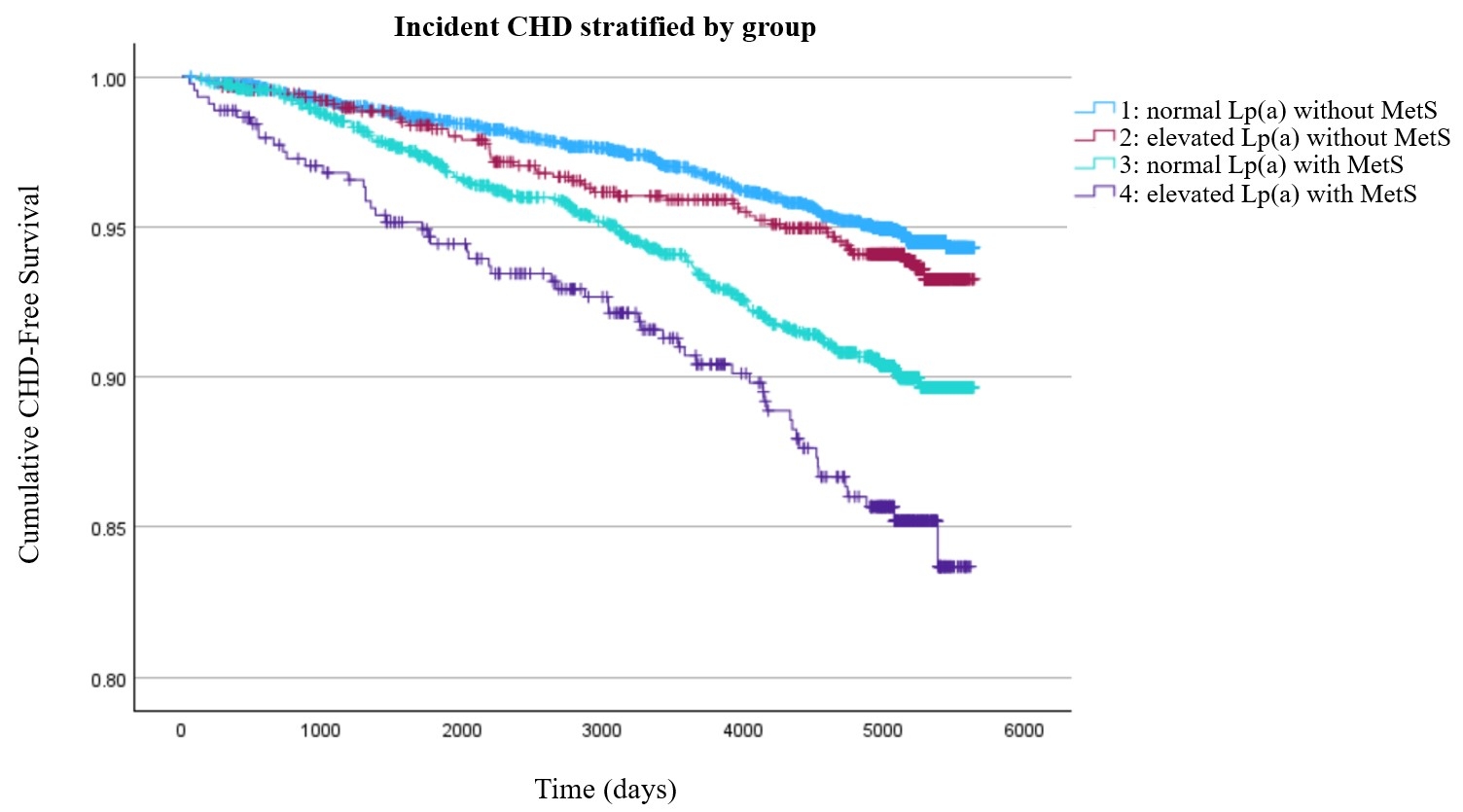
We analyzed 6,664 participants from the MESA (Multiethnic Study of Atherosclerosis) cohort (median follow-up 14.0 years) without baseline CHD. MetS was defined as ≥3 of the following criteria: waist circumference ≥102 cm (men), or ≥88 cm (women), triglycerides ≥150 mg/dL or use of a fibrate medication, HDL-C <40 (men) or <50 (women) or use of a fibrate medication, SBP ≥130 mm Hg and/or DBP ≥85 mm Hg or use of antihypertensive medication, fasting glucose ≥100 mg/dL or use of antidiabetic medication (4). Elevated Lp(a) was defined as a level ≥50 mg/dL. CHD was defined as myocardial infarction, resuscitated cardiac arrest, or CHD death. Participants were divided into four groups: group 1: Normal Lp(a) without MetS, group 2: elevated Lp(a) without MetS, group 3: normal Lp(a) with MetS, group 4: elevated Lp(a) with MetS. Survival analysis using Kaplan-Meier and multivariable Cox proportional hazard models were performed to assess the relationship between Lp(a), MetS, and time to CHD.
Results
In an adjusted model, log [Lp(a)] and MetS were both independently associated with CHD (HR: 1.14; 95% CI: 1.03, 1.25) and (HR: 1.75; 95% CI: 1.35, 2.27). Compared to the reference group (normal Lp(a) without MetS), those with elevated Lp(a) without MetS (group 2) did not have increased risk of CHD (HR: 1.30; 95% CI: 0.94, 1.80). However, those with normal Lp(a) with MetS (group 3) had greater risk of CHD (HR: 1.56; 95% CI: 1.18, 2.05). The highest risk for CHD were in those with elevated Lp(a) with MetS (group 4) (HR: 2.37; 95% CI: 1.66, 3.37).
Conclusions
In this analysis. elevated Lp(a) and MetS independently increase CHD risk. MetS alone significantly increases risk, whereas elevated Lp(a) without MetS does not demonstrate a significant effect. However, their combination confers the highest risk, suggesting a synergistic interaction. These results emphasize the value of assessing Lp(a) in individuals with MetS to improve cardiovascular risk stratification and guide targeted prevention.
Lipoprotein(a) [Lp(a)] and metabolic syndrome (MetS) are well-established risk factors for cardiovascular disease. Recent evidence suggests that high Lp(a) levels may increase the risk of coronary heart disease (CHD) in patients with diabetes, raising the question of whether similar interactions exist between Lp(a) and metabolic syndrome. We aimed to evaluate the joint association of Lp(a) and MetS with incident CHD risk in a large, multi-ethnic, prospective cohort.
Methods
We analyzed 6,664 participants from the MESA (Multiethnic Study of Atherosclerosis) cohort (median follow-up 14.0 years) without baseline CHD. MetS was defined as ≥3 of the following criteria: waist circumference ≥102 cm (men), or ≥88 cm (women), triglycerides ≥150 mg/dL or use of a fibrate medication, HDL-C <40 (men) or <50 (women) or use of a fibrate medication, SBP ≥130 mm Hg and/or DBP ≥85 mm Hg or use of antihypertensive medication, fasting glucose ≥100 mg/dL or use of antidiabetic medication (4). Elevated Lp(a) was defined as a level ≥50 mg/dL. CHD was defined as myocardial infarction, resuscitated cardiac arrest, or CHD death. Participants were divided into four groups: group 1: Normal Lp(a) without MetS, group 2: elevated Lp(a) without MetS, group 3: normal Lp(a) with MetS, group 4: elevated Lp(a) with MetS. Survival analysis using Kaplan-Meier and multivariable Cox proportional hazard models were performed to assess the relationship between Lp(a), MetS, and time to CHD.
Results
In an adjusted model, log [Lp(a)] and MetS were both independently associated with CHD (HR: 1.14; 95% CI: 1.03, 1.25) and (HR: 1.75; 95% CI: 1.35, 2.27). Compared to the reference group (normal Lp(a) without MetS), those with elevated Lp(a) without MetS (group 2) did not have increased risk of CHD (HR: 1.30; 95% CI: 0.94, 1.80). However, those with normal Lp(a) with MetS (group 3) had greater risk of CHD (HR: 1.56; 95% CI: 1.18, 2.05). The highest risk for CHD were in those with elevated Lp(a) with MetS (group 4) (HR: 2.37; 95% CI: 1.66, 3.37).
Conclusions
In this analysis. elevated Lp(a) and MetS independently increase CHD risk. MetS alone significantly increases risk, whereas elevated Lp(a) without MetS does not demonstrate a significant effect. However, their combination confers the highest risk, suggesting a synergistic interaction. These results emphasize the value of assessing Lp(a) in individuals with MetS to improve cardiovascular risk stratification and guide targeted prevention.
More abstracts on this topic:
A Case of Dilated Cardiomyopathy and Systemic Thromboembolism in a Young Patient on Testosterone Replacement Therapy
Sabri Muhammad, Ijaz Naila, Nadeem Ramsha, Checchio Lucy, Riaz Faiza
A Systematic Review and Network Meta-Analysis of Metastatic Castrate-Resistant Prostate Cancer Therapy Cardiotoxicity Given Metastatic Hormone-Sensitive Prostate Cancer Treatment HistoryAziz Moez, Swaby Justin, Deng Brett, Hartshorne Taylor, Desai Shubh, Zhang Allan, Xiao Daniel, Sanchez Darren, Imber Jared, Song Jeffrey, Rivas Alexis, Molony Donald, Guhan Maya, Ranganath Shreyas, Jacob Jerril, Ziaolhagh Ali, Ali Abdelrahman, Yusuf Syed, Canfield Steven, Iliescu Cezar, Monlezun Dominique, Higgason Noel, Brunckhorst Oliver, Roland Jerry, Owen Christopher, Iacobucci Alexander Samuel, Galan Jacob