Final ID: MP2663
Cardiac Sympathetic Denervation, Catheter and Surgical Hybrid Ablation Successfully Treat Refractory Ventricular Arrhythmias – a Comprehensive Heart Team Approach
Abstract Body (Do not enter title and authors here): Background: Although percutaneous ablation is currently the mainstay of ventricular arrhythmia (VA) management, surgical cardiac sympathetic denervation (CSD) as well as surgical epicardial ablation (SEA) complement the comprehensive management of refractory VA.
Hypothesis: Surgical/hybrid interventions can safely and effectively treat refractory VA across the full spectrum of VA etiologies and complexities.
Methods: We retrospectively identified 19 patients with refractory VA who underwent CSD and/or SEA, in the form of radiofrequency ablation or intramyocardial direct alcohol injection using thoracoscopy or thoracotomy at a single institution between 2007 and 2024. Patient demographics were collected and correlated with post-operative ventricular tachycardia (VT)-free survival.
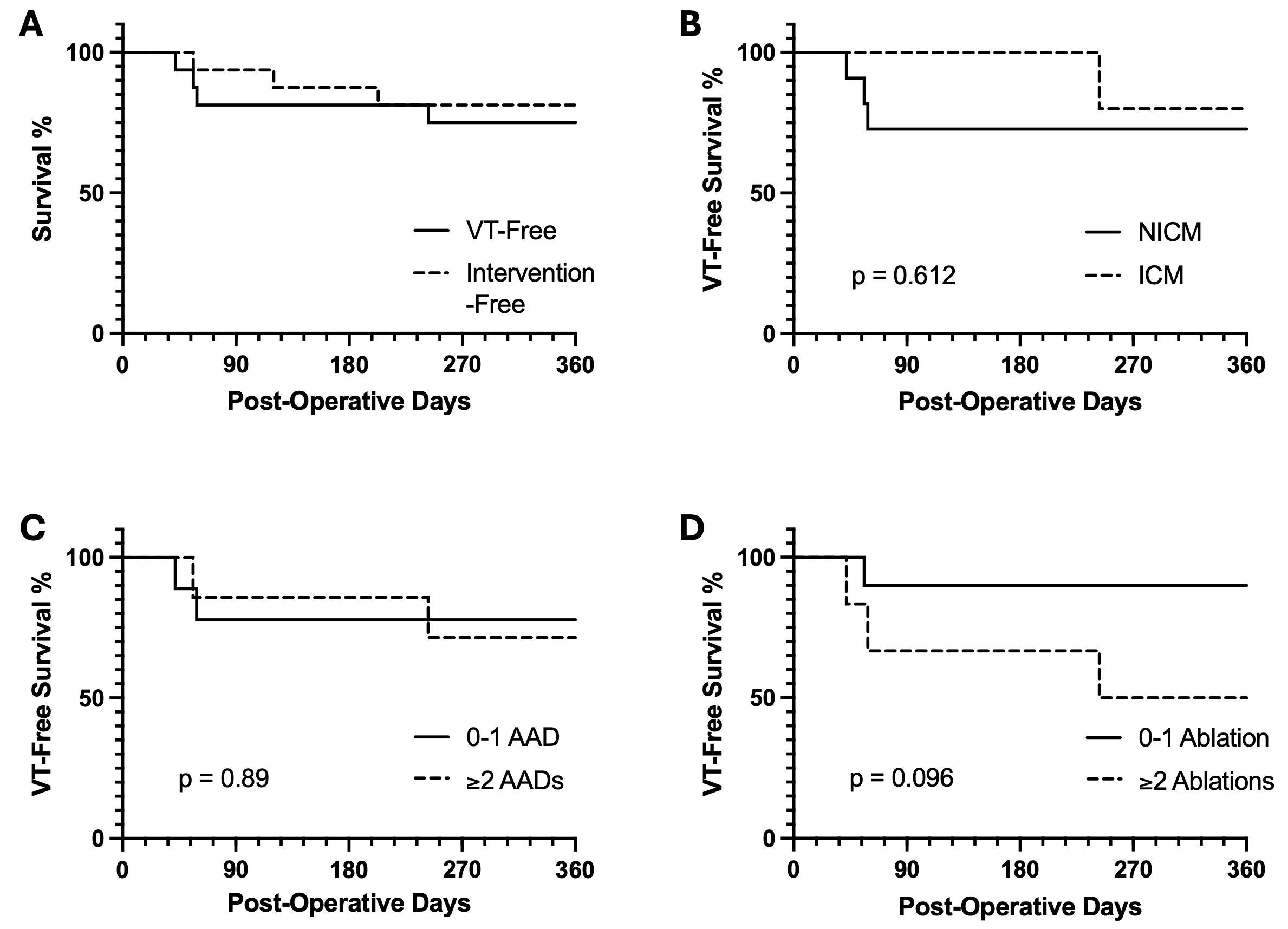
Results: 19 male patients underwent a surgical/hybrid intervention with a median age 63, 74% non-ischemic VA etiology, average of 2 failed anti-arrhythmic drugs (AAD), average of 2 endocardial and 1 epicardial VT ablations prior to surgery. 13 patients underwent CSD, 4 SEA and 2 both. Three patients were excluded from quantitative analyses due to incomplete data. At one-year post-operative analysis, 75% of patients were free from VT and 81% free from reintervention (Figure 1A). All VT recurrences were seen in CSD-only patients, with all but one occurring within 60 days post-CSD and one late recurrence on day 243. VT-free survival did not differ in patients stratified by VA etiology (non-ischemic vs ischemic, 27% vs 20%, p = 0.612, 1B), number of failed AAD (0-1 vs ≥2, 22% vs 29%, p = 0.89, 1C) or number of prior ablations (0-1 vs ≥2, 10% vs 50%, p = 0.096, 1D). Seattle Heart Failure Model (SHFM) score (mean 0.26 ±0.72) or PAINESD score (mean 8 ±7) did not predict VT-free survival (R2 = 0.01, p = 0.68 and R2 = 0.07, p = 0.33 respectively).
Conclusions: CSD and SEA are extremely effective in treating refractory VA. CSD might require up to 60 days to take full effect but provides excellent long-term outcomes. Indicators of disease severity did not correlate with clinical success and high-risk patients identified by SHFM and PAINESD scores still benefited from surgical hybrid intervention. This suggests that most patients suffering from refractory VA can benefit from CSD and SEA.
Hypothesis: Surgical/hybrid interventions can safely and effectively treat refractory VA across the full spectrum of VA etiologies and complexities.
Methods: We retrospectively identified 19 patients with refractory VA who underwent CSD and/or SEA, in the form of radiofrequency ablation or intramyocardial direct alcohol injection using thoracoscopy or thoracotomy at a single institution between 2007 and 2024. Patient demographics were collected and correlated with post-operative ventricular tachycardia (VT)-free survival.
Results: 19 male patients underwent a surgical/hybrid intervention with a median age 63, 74% non-ischemic VA etiology, average of 2 failed anti-arrhythmic drugs (AAD), average of 2 endocardial and 1 epicardial VT ablations prior to surgery. 13 patients underwent CSD, 4 SEA and 2 both. Three patients were excluded from quantitative analyses due to incomplete data. At one-year post-operative analysis, 75% of patients were free from VT and 81% free from reintervention (Figure 1A). All VT recurrences were seen in CSD-only patients, with all but one occurring within 60 days post-CSD and one late recurrence on day 243. VT-free survival did not differ in patients stratified by VA etiology (non-ischemic vs ischemic, 27% vs 20%, p = 0.612, 1B), number of failed AAD (0-1 vs ≥2, 22% vs 29%, p = 0.89, 1C) or number of prior ablations (0-1 vs ≥2, 10% vs 50%, p = 0.096, 1D). Seattle Heart Failure Model (SHFM) score (mean 0.26 ±0.72) or PAINESD score (mean 8 ±7) did not predict VT-free survival (R2 = 0.01, p = 0.68 and R2 = 0.07, p = 0.33 respectively).
Conclusions: CSD and SEA are extremely effective in treating refractory VA. CSD might require up to 60 days to take full effect but provides excellent long-term outcomes. Indicators of disease severity did not correlate with clinical success and high-risk patients identified by SHFM and PAINESD scores still benefited from surgical hybrid intervention. This suggests that most patients suffering from refractory VA can benefit from CSD and SEA.
More abstracts on this topic:
4D Cardiac Optogenetics Enable Complex Arrhythmia Modelling and Precise Interventional Simulation
Wexler Yehuda, Grinstein Harel, Landesberg Michal, Glatstein Shany, Huber Irit, Arbel Gil, Gepstein Lior
A Bifunctional Actuator Reverses NaV1.5 Dysfunction Linked To Cardiac ArrhythmiasFossier Lucile, Yehya Marc, Mahling Ryan, Gabelli Sandra, Colecraft Henry, Ben Johny Manu