Final ID: Su4098
Association Between Novel Arterial Wall Atherogenesis Markers With Incident Myocardial Infarction: Observations From The Dallas Heart Study
Abstract Body (Do not enter title and authors here): Background: Although traditional risk factors and chronic inflammation are drivers of coronary artery disease (CAD), risk factors and circulating inflammation markers do not fully capture those at risk for myocardial infarction (MI). This is likely due to their non-specific nature and inability to accurately capture atherogenesis potential at the arterial wall. To address these gaps, we developed an ex vivo arterial wall model that can determine atherogenesis potential testing a person’s plasma in assays that directly reflect key early steps of atherosclerosis. In this study, we aimed to demonstrate clinical relevance of these arterial wall markers with incident MI.
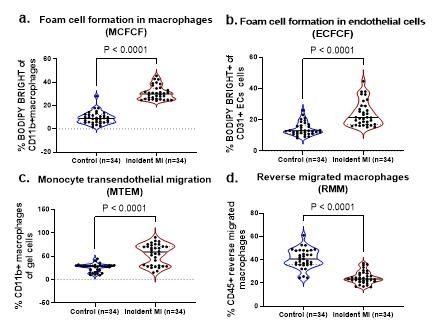
Method: In a nested case-control study, 34 incident myocardial infarction (MI) cases and 34 controls (matched for age, sex, and race/ethnicity) were selected from the Dallas Heart Study (a community-based cohort, >3,000 participants without prevalent CAD at baseline). Using stored plasma from participants at baseline, single-cell flow cytometry, and standardized peripheral blood mononuclear cells (pBMCs), atherogenesis phenotypes were assessed by 1) monocyte subset profile; 2) % monocyte transendothelial migration (MTEM) and % reverse migration of macrophages (RMM) using TNF-alpha stimulated endothelial cells and pBMCs in collagen gels over 48 hours; and 3) % foam cell formation in endothelial cells (ECFCF), and macrophages (MCFCF) using BODIPY cholesterol.
Results: Mean age was 58 years (49% women, 66% Black, and 9% Hispanic). We found lower classical monocytes (% CD14+CD16-: 7.7 vs 9.5; p=0.018, higher pro-inflammatory monocytes (% CD14dimCD16+: 8.9 vs 2.6; % CD14++CD16+: 5.7 vs 1.2; p<0.0001), higher foam cell formation (% MCFCF: 30.1 vs 9.0; % ECFCF: 21.5 vs 12.9; p<0.0001) and higher MTEM (59.5% vs 28.8%; p<0.0001) in incident MI cases vs controls. Further, RMM (23.4% vs 40.7%; p<0.0001) was reduced in incident MI cases vs controls. Our findings suggest these inflammatory parameters of atherogenesis are accurate MI risk predictors.
Conclusion: Our study demonstrated that arterial wall markers of atherogenesis measured at baseline when disease-free are accurate predictors of incident MI risk. These arterial wall markers may serve as ideal candidates to accurately assess risk, monitor therapy, and test novel therapeutic agents to lower the burden of coronary artery disease. These findings require external validation and assessment in response to therapies to determine clinical potential.
Method: In a nested case-control study, 34 incident myocardial infarction (MI) cases and 34 controls (matched for age, sex, and race/ethnicity) were selected from the Dallas Heart Study (a community-based cohort, >3,000 participants without prevalent CAD at baseline). Using stored plasma from participants at baseline, single-cell flow cytometry, and standardized peripheral blood mononuclear cells (pBMCs), atherogenesis phenotypes were assessed by 1) monocyte subset profile; 2) % monocyte transendothelial migration (MTEM) and % reverse migration of macrophages (RMM) using TNF-alpha stimulated endothelial cells and pBMCs in collagen gels over 48 hours; and 3) % foam cell formation in endothelial cells (ECFCF), and macrophages (MCFCF) using BODIPY cholesterol.
Results: Mean age was 58 years (49% women, 66% Black, and 9% Hispanic). We found lower classical monocytes (% CD14+CD16-: 7.7 vs 9.5; p=0.018, higher pro-inflammatory monocytes (% CD14dimCD16+: 8.9 vs 2.6; % CD14++CD16+: 5.7 vs 1.2; p<0.0001), higher foam cell formation (% MCFCF: 30.1 vs 9.0; % ECFCF: 21.5 vs 12.9; p<0.0001) and higher MTEM (59.5% vs 28.8%; p<0.0001) in incident MI cases vs controls. Further, RMM (23.4% vs 40.7%; p<0.0001) was reduced in incident MI cases vs controls. Our findings suggest these inflammatory parameters of atherogenesis are accurate MI risk predictors.
Conclusion: Our study demonstrated that arterial wall markers of atherogenesis measured at baseline when disease-free are accurate predictors of incident MI risk. These arterial wall markers may serve as ideal candidates to accurately assess risk, monitor therapy, and test novel therapeutic agents to lower the burden of coronary artery disease. These findings require external validation and assessment in response to therapies to determine clinical potential.
More abstracts on this topic:
9p21.3 variants drive coronary calcification by suppressing statherin expression
Soheili Fariborz, Almontashiri Naif, Heydarikhorneh Niloufar, Vilmundarson Ragnar, Chen Hsiao-huei, Stewart Alexandre
84 Immune checkpoint profiling in major aortic diseases leads to identification of potential roles of CD155-CD206 pathway in suppressing inflammation and immune responsesShao Ying, Saaoud Fatma, Xu Keman, Lu Yifan, Jiang Xiaohua, Wang Hong, Yang Xiaofeng