Final ID: MP2044
GLP-1 Analogues and Cardiovascular Outcomes in Heart Failure Patients: A Network Meta-Analysis
Abstract Body (Do not enter title and authors here):
Background:
Heart failure affects over 56 million globally, with sodium-glucose cotransporter-2 (SGLT2) inhibitors now integral to guideline-directed therapy. While glucagon-like peptide-1 receptor agonists (GLP-1 RAs) show promise for heart failure event reduction, their comparative effectiveness on heart failure-specific outcomes remains unclear. This study aimed to evaluate and rank the comparative effectiveness of different GLP-1 RAs on major adverse cardiovascular events (MACE), heart failure hospitalization, and cardiovascular (CV) mortality in patients with heart failure.
Methods:
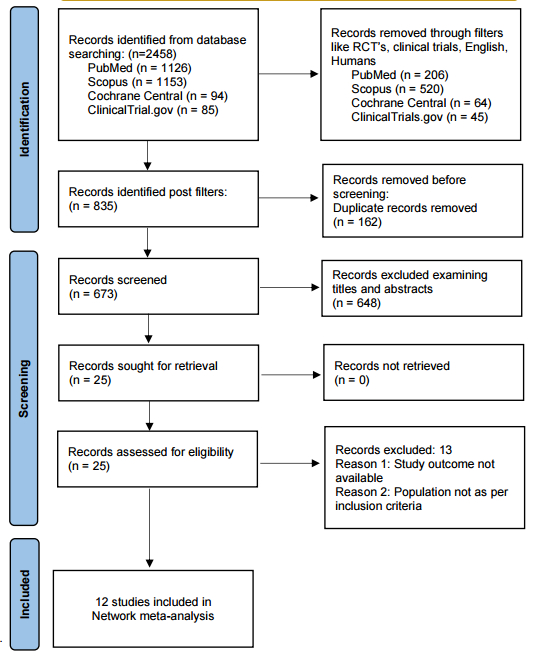
We systematically searched PubMed, Scopus, Cochrane Central, and ClinicalTrials.gov through May, 2025. A pairwise network meta-analysis using a random effects model compared GLP-1 RAs (Albiglutide, Dulaglutide, Exenatide, Liraglutide, Lixisenatide, Semaglutide, Tirzepatide) to placebo, assessing relative risk and P-scores for efficacy ranking was performed on R programming.
Results:
Twelve randomized controlled trials with 15,761 heart failure patients were included (mean age 64 years, follow-up 24-280 weeks).
For MACE, no drug showed a significant effect. However, Albiglutide had the highest P-score of 0.77, followed by Dulaglutide (0.59) and Semaglutide (0.54) with heterogeneity I2 = 55.9%, p = 0.10.
For heart failure hospitalizations, heterogeneity was low (I2 = 22.7%, p = 0.27). Tirzepatide ranked highest and was statistically significant in reducing hospitalization (RR: 0.47; 95% CI: 0.23-0.93; P-score: 0.96). Other GLP1-RAs showed no significant effects, with Semaglutide (P-score: 0.71) and Dulaglutide (0.67) ranking next.
For CV mortality, no heterogeneity was observed (I2 = 0%, p = 0.62). Semaglutide significantly reduced risk (RR: 0.72; 95% CI: 0.57-0.89; P-score: 0.92), followed by Liraglutide (0.67) and Dulaglutide (0.61). Exenatide and Tirzepatide showed no benefit at all.
Conclusion:
In HF patients, GLP-1 RAs differ in their cardiovascular benefit profiles. Tirzepatide demonstrated maximum benefit in reducing HF hospitalizations, and Semaglutide showed promising results in lowering CV mortality; however no therapy appeared to be effective for MACE. These findings support personalized GLP-1 RAs selection based on patient-specific cardiovascular risk profiles and treatment priorities in comprehensive heart failure management. Future trials directly comparing various GLP-1 RAs in heart failure phenotypes (HFrEF/HFpEF) are needed to validate differential outcome benefits.
Background:
Heart failure affects over 56 million globally, with sodium-glucose cotransporter-2 (SGLT2) inhibitors now integral to guideline-directed therapy. While glucagon-like peptide-1 receptor agonists (GLP-1 RAs) show promise for heart failure event reduction, their comparative effectiveness on heart failure-specific outcomes remains unclear. This study aimed to evaluate and rank the comparative effectiveness of different GLP-1 RAs on major adverse cardiovascular events (MACE), heart failure hospitalization, and cardiovascular (CV) mortality in patients with heart failure.
Methods:
We systematically searched PubMed, Scopus, Cochrane Central, and ClinicalTrials.gov through May, 2025. A pairwise network meta-analysis using a random effects model compared GLP-1 RAs (Albiglutide, Dulaglutide, Exenatide, Liraglutide, Lixisenatide, Semaglutide, Tirzepatide) to placebo, assessing relative risk and P-scores for efficacy ranking was performed on R programming.
Results:
Twelve randomized controlled trials with 15,761 heart failure patients were included (mean age 64 years, follow-up 24-280 weeks).
For MACE, no drug showed a significant effect. However, Albiglutide had the highest P-score of 0.77, followed by Dulaglutide (0.59) and Semaglutide (0.54) with heterogeneity I2 = 55.9%, p = 0.10.
For heart failure hospitalizations, heterogeneity was low (I2 = 22.7%, p = 0.27). Tirzepatide ranked highest and was statistically significant in reducing hospitalization (RR: 0.47; 95% CI: 0.23-0.93; P-score: 0.96). Other GLP1-RAs showed no significant effects, with Semaglutide (P-score: 0.71) and Dulaglutide (0.67) ranking next.
For CV mortality, no heterogeneity was observed (I2 = 0%, p = 0.62). Semaglutide significantly reduced risk (RR: 0.72; 95% CI: 0.57-0.89; P-score: 0.92), followed by Liraglutide (0.67) and Dulaglutide (0.61). Exenatide and Tirzepatide showed no benefit at all.
Conclusion:
In HF patients, GLP-1 RAs differ in their cardiovascular benefit profiles. Tirzepatide demonstrated maximum benefit in reducing HF hospitalizations, and Semaglutide showed promising results in lowering CV mortality; however no therapy appeared to be effective for MACE. These findings support personalized GLP-1 RAs selection based on patient-specific cardiovascular risk profiles and treatment priorities in comprehensive heart failure management. Future trials directly comparing various GLP-1 RAs in heart failure phenotypes (HFrEF/HFpEF) are needed to validate differential outcome benefits.
More abstracts on this topic:
A Novel Machine Learning-based Adverse Cardiovascular Events Risk Algorithm For Cancer Patients Treated With Tyrosine Kinase Inhibitors
Wahi Shawn, Cross James, Mora Ruben, Im Yunju, Kwan Jennifer
5-oxoproline/ OPLAH Axis Alleviates Doxorubicin-induced Cardiomyopathy By Inhibiting FerroptosisJiang Meng, Guo Xinning