Final ID: MP1365
Association Between Myocardial Lipomatous Metaplasia And Sudden Cardiac Death In Patients With Prior Myocardial Infarction
Abstract Body (Do not enter title and authors here): Objective
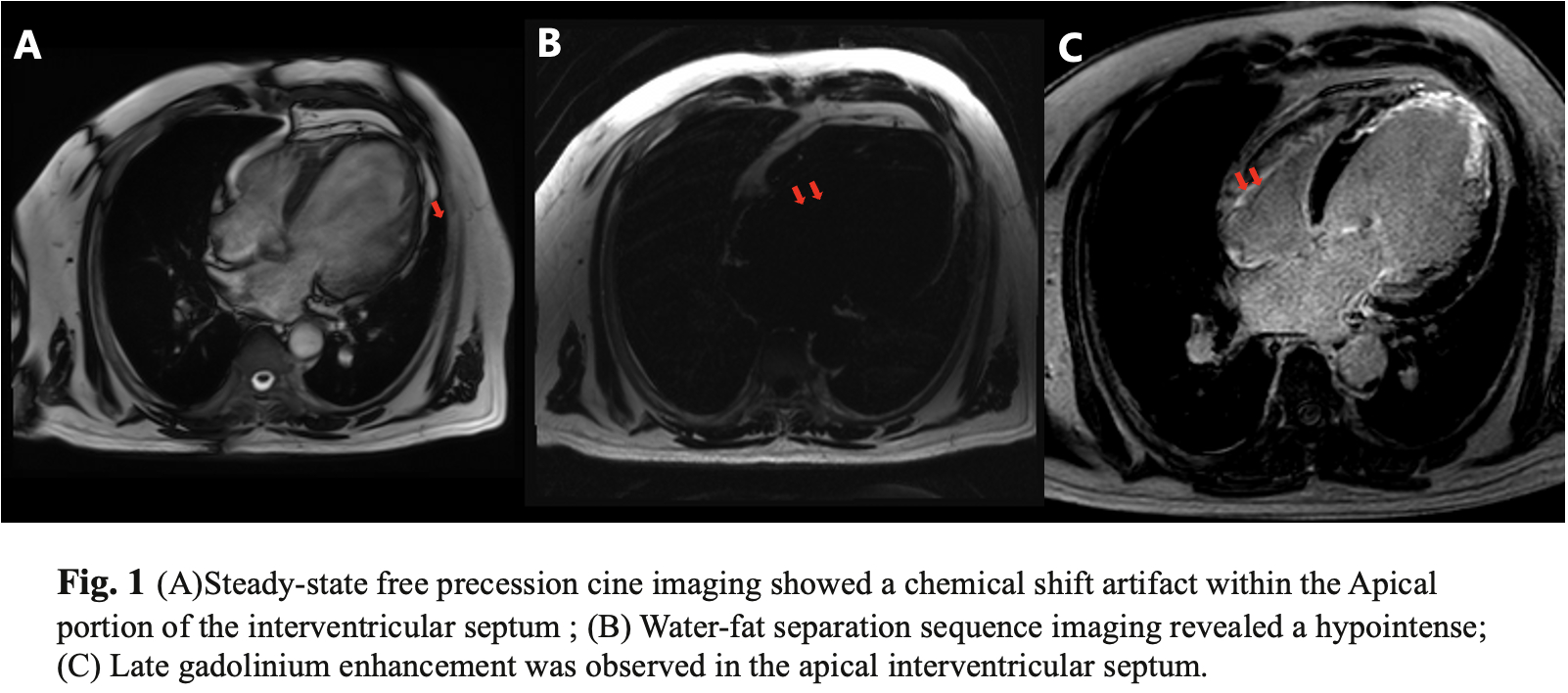
Infarcted myocardium can be infiltrated by adipose cells, known as lipomatous metaplasia (LM). It has been suggested that LM may provide a substrate for post-infarct ventricular tachycardia (VT). This study aims to noninvasively characterize the prevalence of LM using late gadolinium enhancement cardiac magnetic resonance (LGE-CMR) and explore the association between LM and sudden cardiac death (SCD) events in patients with prior myocardial infarction (PMI). (Figure 1 in the Appendix)
Methods
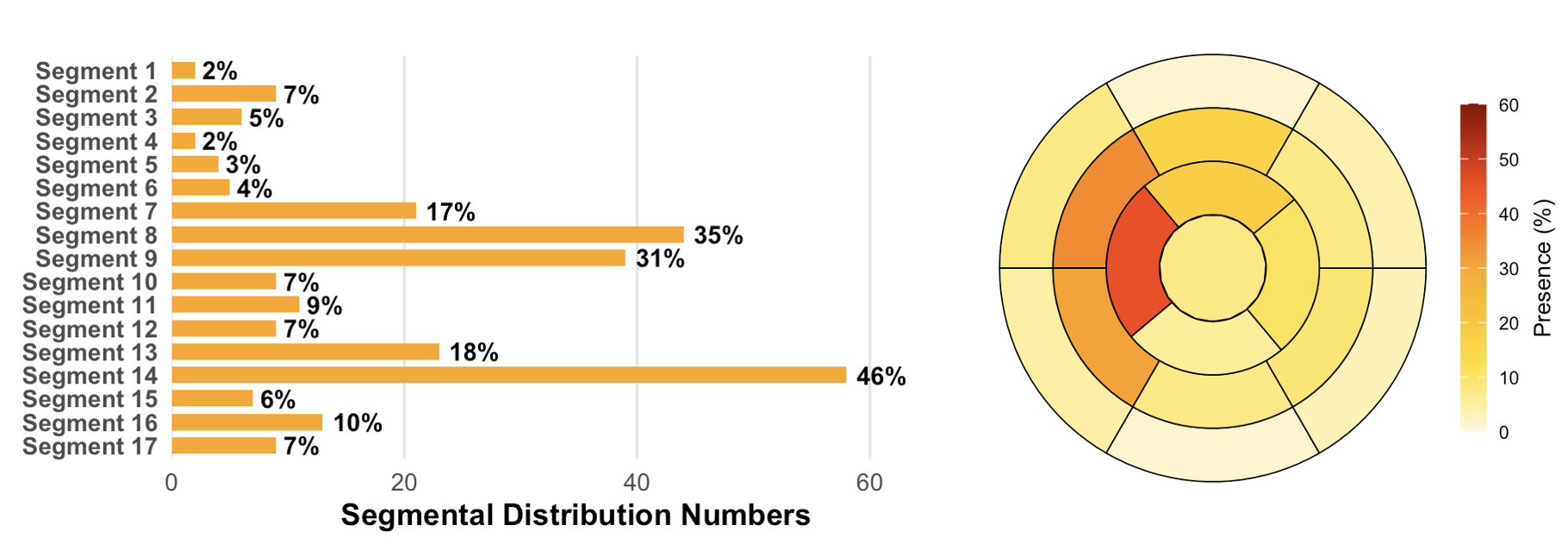
A total of 896 patients with PMI were retrospective analyzed. PMI was confirmed by CMR evidence of subendocardial or transmural LGE in a coronary artery-specific distribution. The extent of infarct size and the presence of LM within infarcted myocardium were recorded. (Figure 2 in the Appendix) All patients were followed up for SCD and surrogate events, including resuscitated cardiac arrest and appropriate discharges from an implantable defibrillator.
Results
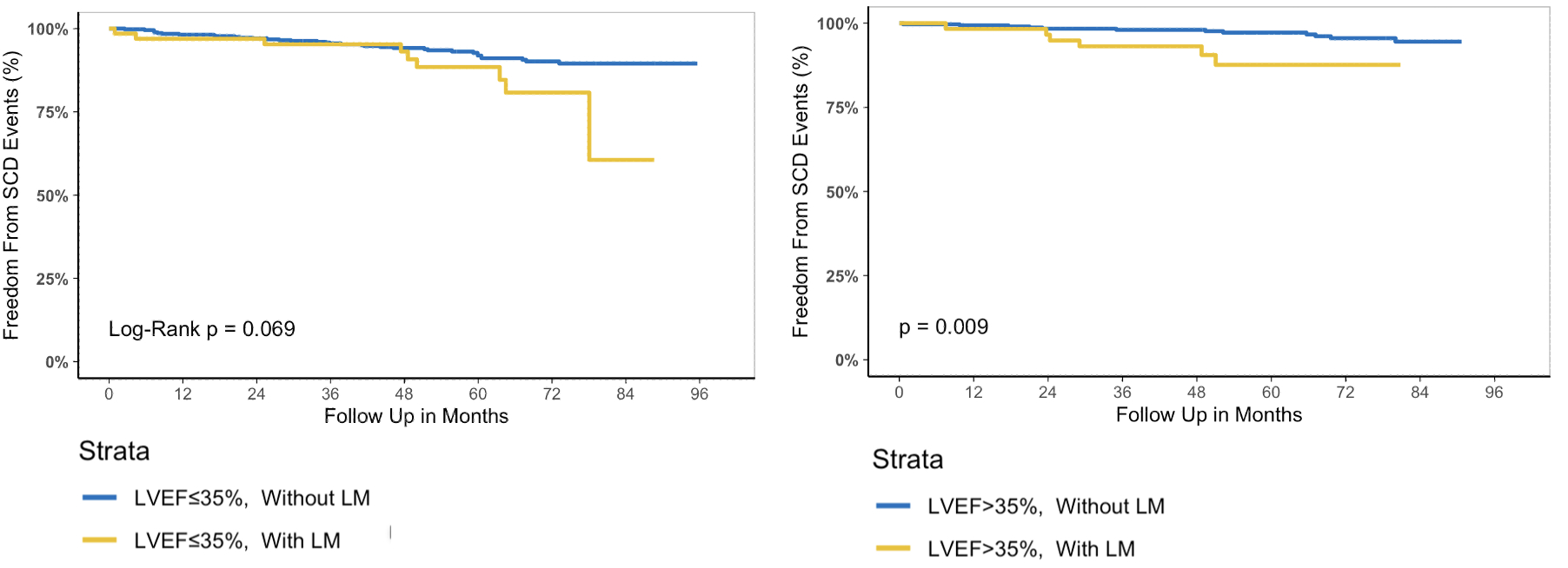
A total of 896 patients with PMI were included (mean age 56.3 ± 10.7 years;88.4% Male), LM was detected in 127 (14.2%) patients. During a median follow-up of 64months, 62 (6.9%) patients experienced SCD events. Patients with LM demonstrated a significantly higher extent of LGE involvement (19.9 ± 11.9% vs. 23.4 ± 9.1%, P < 0.001) and higher SCD events (11.8% VS 6.1%, P=0.035) compared to those without LM. Multivariable Cox regression analysis, adjusted for LGE%, EDVi, and NT-proBNP, demonstrated that LM was independently associated with SCD events (HR=2.51, 95% CI: 1.38-4.56, p=0.002). When LM was combined with the conventional model (LVEF≤35%), the prognostic performance of the model was improved (C-index 0.58 vs 0.62, p<0.05). Furthermore, in the subgroup of patients with LVEF>35%, the Kaplan-Meier survival analysis revealed that those with LM had significantly worse SCD-free survival compared to those without LM (p=0.009). (Figure 3 in the Appendix)
Conclusion
In patients with PMI, the presence of LM was independently associated with SCD risk. Furthermore, this association persisted in patients with LVEF >35%, indicating LM may serve as a new marker for SCD risk stratification.
Infarcted myocardium can be infiltrated by adipose cells, known as lipomatous metaplasia (LM). It has been suggested that LM may provide a substrate for post-infarct ventricular tachycardia (VT). This study aims to noninvasively characterize the prevalence of LM using late gadolinium enhancement cardiac magnetic resonance (LGE-CMR) and explore the association between LM and sudden cardiac death (SCD) events in patients with prior myocardial infarction (PMI). (Figure 1 in the Appendix)
Methods
A total of 896 patients with PMI were retrospective analyzed. PMI was confirmed by CMR evidence of subendocardial or transmural LGE in a coronary artery-specific distribution. The extent of infarct size and the presence of LM within infarcted myocardium were recorded. (Figure 2 in the Appendix) All patients were followed up for SCD and surrogate events, including resuscitated cardiac arrest and appropriate discharges from an implantable defibrillator.
Results
A total of 896 patients with PMI were included (mean age 56.3 ± 10.7 years;88.4% Male), LM was detected in 127 (14.2%) patients. During a median follow-up of 64months, 62 (6.9%) patients experienced SCD events. Patients with LM demonstrated a significantly higher extent of LGE involvement (19.9 ± 11.9% vs. 23.4 ± 9.1%, P < 0.001) and higher SCD events (11.8% VS 6.1%, P=0.035) compared to those without LM. Multivariable Cox regression analysis, adjusted for LGE%, EDVi, and NT-proBNP, demonstrated that LM was independently associated with SCD events (HR=2.51, 95% CI: 1.38-4.56, p=0.002). When LM was combined with the conventional model (LVEF≤35%), the prognostic performance of the model was improved (C-index 0.58 vs 0.62, p<0.05). Furthermore, in the subgroup of patients with LVEF>35%, the Kaplan-Meier survival analysis revealed that those with LM had significantly worse SCD-free survival compared to those without LM (p=0.009). (Figure 3 in the Appendix)
Conclusion
In patients with PMI, the presence of LM was independently associated with SCD risk. Furthermore, this association persisted in patients with LVEF >35%, indicating LM may serve as a new marker for SCD risk stratification.
More abstracts on this topic:
A Case of Steroid-Refractory Immune-checkpoint-inhibitor Induced Myocarditis Responsive to Mycophenolate and Anti-thymocyte globulin
Dabdoub Jorge, Wilson Michael, Gottbrecht Matthew, Salazar Ryan, Shih Jeffrey
Benchmarking the Impact of Out-of-Hospital Cardiac Arrest Treatment on All-Cause Mortality in the United StatesNeumar Robert, Mcnally Bryan, Wiebe Douglas