Final ID: Sa1014
Fungal Pericarditis Masquerading as Sterile Effusion: A Case of Delayed Recognition
Abstract Body (Do not enter title and authors here): Background:
Fungal pericarditis is rare, accounting for <1% of pericardial effusions. Up to 50% of cases occur in immunocompetent individuals. Overall, 30% of cases present without systemic involvement1. It is often underdiagnosed, leading to high mortality (50%) from delayed treatment 2. Prompt recognition, antifungal therapy, and surgical intervention are keys to improving outcomes.
Case:
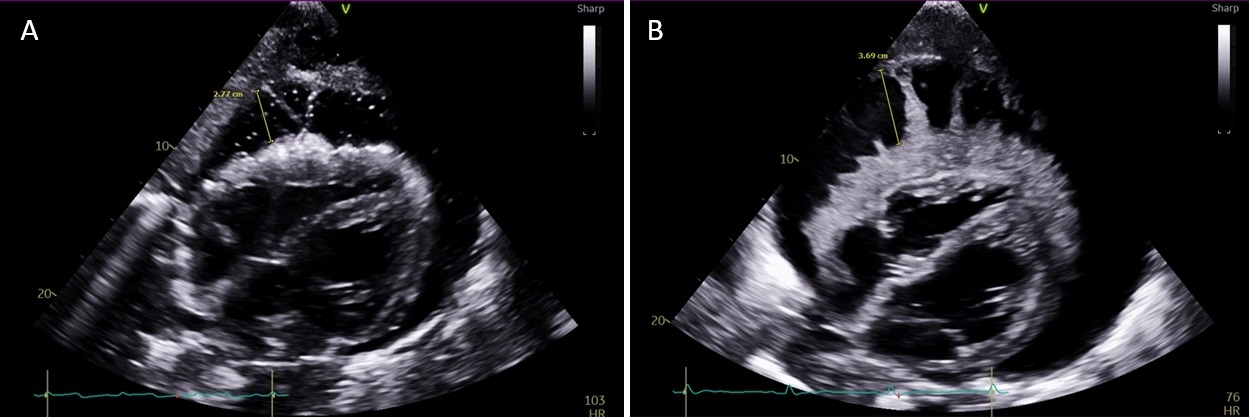
A 36-year-old male with methamphetamine-induced heart failure, esophageal stricture, cachexia, and esophageal candidiasis presented with chest pain after blunt chest trauma. Chest CT showed multifocal pneumonia and a large pericardial effusion with pneumopericardium. TTE revealed a loculated pericardial effusion without tamponade and a thick epicardial rind (Fig. 1A). Pericardiocentesis yielded 40 mL of yellow, gelatinous, acellular fluid.
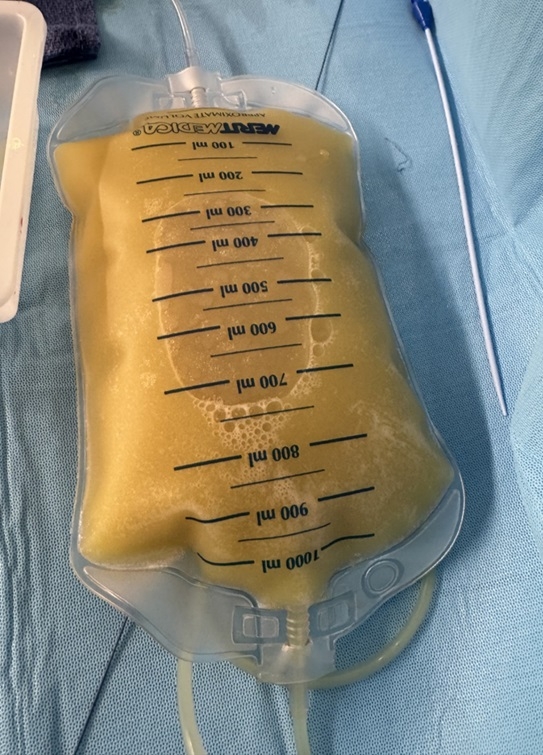
Later in the admission, he became hypotensive requiring vasopressors. Repeat TTE showed a very large effusion with tamponade physiology and new fingerlike tendrils on the epicardial surface (Fig. 1B). He was transferred for urgent pericardiocentesis with removal of 1.4 L of turbid, yellow-opaque fluid resulting in hemodynamic improvement (Fig. 2). Initial fluid studies were non-diagnostic and sterile. However, culture eventually grew Candida albicans and he began treatment with micafungin.
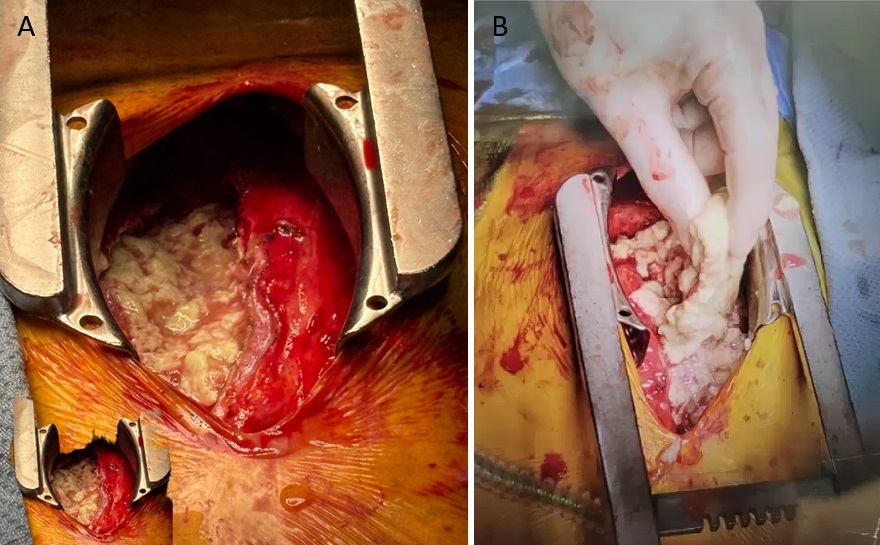
Although prior esophageal candidiasis raised concern for a fistula, this was ruled out by normal pericardial amylase and CT esophagram as well as gastrografin swallow esophagram. Due to continued drain output and persistent effusion on follow-up TTEs, he underwent surgical debridement. Dense, white, rubbery material was removed from the pericardial space (Fig. 3A and 3B). Postoperatively, he recovered well and was discharged to acute rehab.
Discussion:
This case highlights the diagnostic challenge of fungal pericarditis, especially in immunocompetent hosts. Though our patient was not overtly immunocompromised, his history of esophageal candidiasis suggests impairment of his immune system. The initial acellular, culture-negative effusion mimicked a sterile process. When imaging and clinical findings conflict, multidisciplinary evaluation is critical. Early recognition and aggressive source control are essential in managing this rare, highly lethal condition.
Fungal pericarditis is rare, accounting for <1% of pericardial effusions. Up to 50% of cases occur in immunocompetent individuals. Overall, 30% of cases present without systemic involvement1. It is often underdiagnosed, leading to high mortality (50%) from delayed treatment 2. Prompt recognition, antifungal therapy, and surgical intervention are keys to improving outcomes.
Case:
A 36-year-old male with methamphetamine-induced heart failure, esophageal stricture, cachexia, and esophageal candidiasis presented with chest pain after blunt chest trauma. Chest CT showed multifocal pneumonia and a large pericardial effusion with pneumopericardium. TTE revealed a loculated pericardial effusion without tamponade and a thick epicardial rind (Fig. 1A). Pericardiocentesis yielded 40 mL of yellow, gelatinous, acellular fluid.
Later in the admission, he became hypotensive requiring vasopressors. Repeat TTE showed a very large effusion with tamponade physiology and new fingerlike tendrils on the epicardial surface (Fig. 1B). He was transferred for urgent pericardiocentesis with removal of 1.4 L of turbid, yellow-opaque fluid resulting in hemodynamic improvement (Fig. 2). Initial fluid studies were non-diagnostic and sterile. However, culture eventually grew Candida albicans and he began treatment with micafungin.
Although prior esophageal candidiasis raised concern for a fistula, this was ruled out by normal pericardial amylase and CT esophagram as well as gastrografin swallow esophagram. Due to continued drain output and persistent effusion on follow-up TTEs, he underwent surgical debridement. Dense, white, rubbery material was removed from the pericardial space (Fig. 3A and 3B). Postoperatively, he recovered well and was discharged to acute rehab.
Discussion:
This case highlights the diagnostic challenge of fungal pericarditis, especially in immunocompetent hosts. Though our patient was not overtly immunocompromised, his history of esophageal candidiasis suggests impairment of his immune system. The initial acellular, culture-negative effusion mimicked a sterile process. When imaging and clinical findings conflict, multidisciplinary evaluation is critical. Early recognition and aggressive source control are essential in managing this rare, highly lethal condition.
More abstracts on this topic:
A Novel Cardiac Simulator "ped UT-Heart" to Support Decision-Making in Surgical Procedures for Complex Congenital Heart Disease
Shiraishi Isao, Kurosaki Kenichi, Iwai Shigemitsu, Washio Takumi, Sugiura Seiryo, Hisada Toshiaki
An Unusual Presentation of Cerebellar Stroke Following the Removal of Microaxial Flow PumpLiu Zi Qian, Alsheikh-kassim Mohammad, Karpenos Joseph, Frodey Kevin