Final ID: MP2433
Penicillin Prophylaxis and Adherence in Latent Rheumatic Heart Disease: Systematic Review and Metaanalysis of Outcomes
Abstract Body (Do not enter title and authors here):
Background
Although Rheumatic Heart Disease prevalence has declined in high-income countries, it remains a major cause of morbidity and mortality in low-income areas. The 2012 WHF criteria define latent RHD (LRHD) as subclinical valvular lesions without classical RHD symptoms. LRHD may progress, persist, or regress, and the benefit of echocardiographic screening followed by penicillin prophylaxis remains unclear. For that reason, we developed a meta-analysis to investigate the effects of the penicillin prophylaxis, its adherence, and the outcomes on LRHD.
Hypothesis
Does penicillin prophylaxis reduce LRHD progression, persistence, or regression?
Does adherence affect these outcomes?
Methods
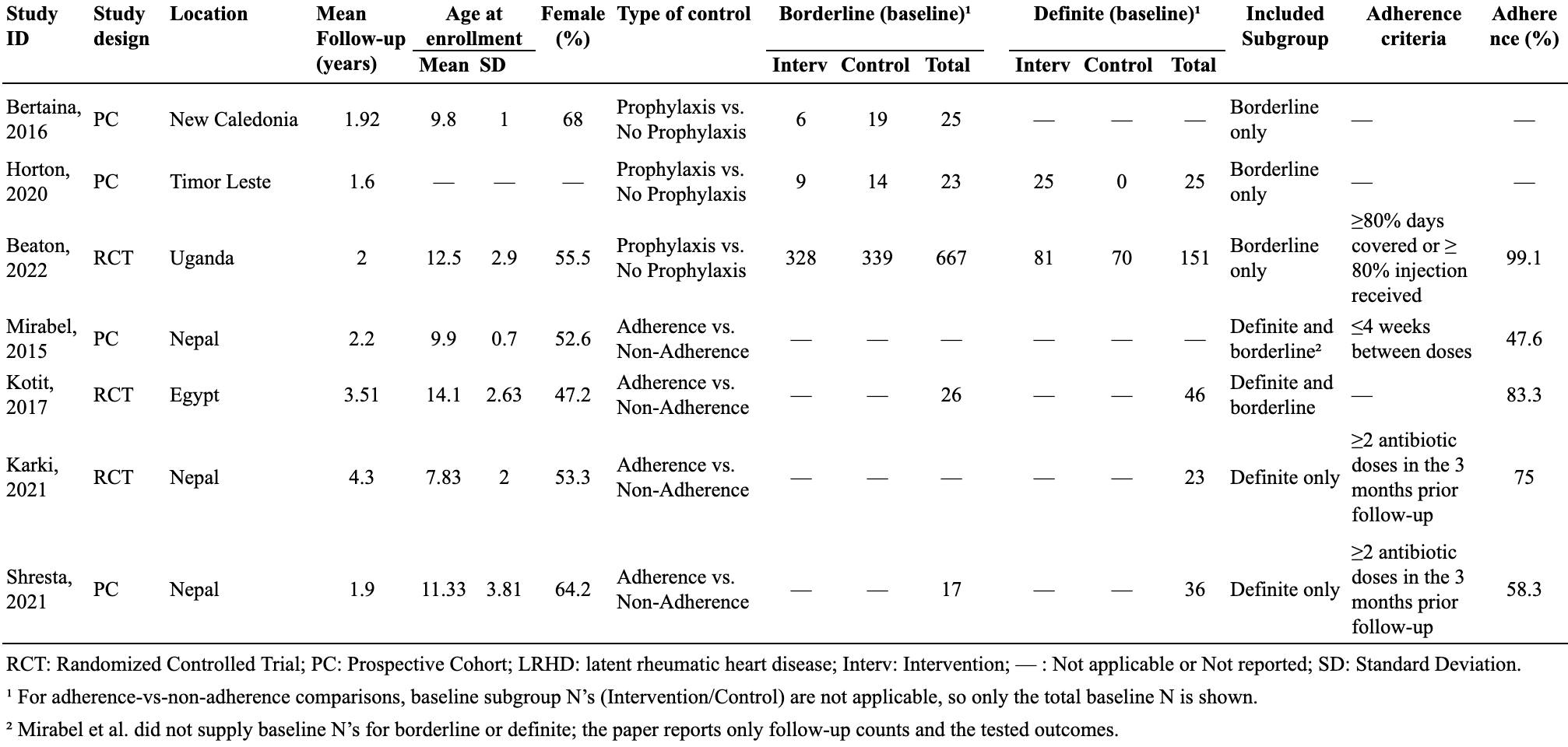
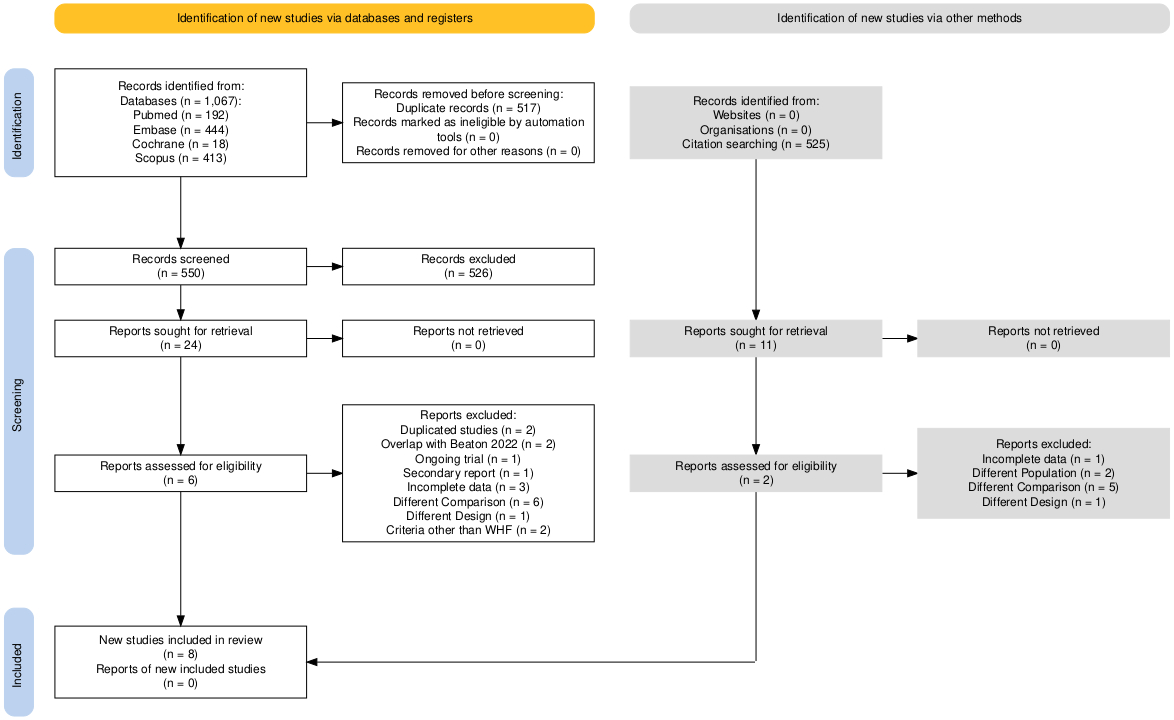
Following PRISMA and registered in PROSPERO (CRD420251012711), we searched PubMed, Embase, CENTRAL, and Scopus through February 18, 2025. Included studies compared prophylaxis versus no prophylaxis or adherent versus non-adherent LRHD patients (WHF 2012). Seven studies (n = 940; three RCTs, four cohorts) were included. Data extracted included event counts for progression, persistence, and regression. Risk of bias was assessed with RoB 2 and ROBINS-I. Random-effects REML models in Stata pooled log risk ratios (log RR) with 95 % CIs; heterogeneity was quantified by I2.
Results
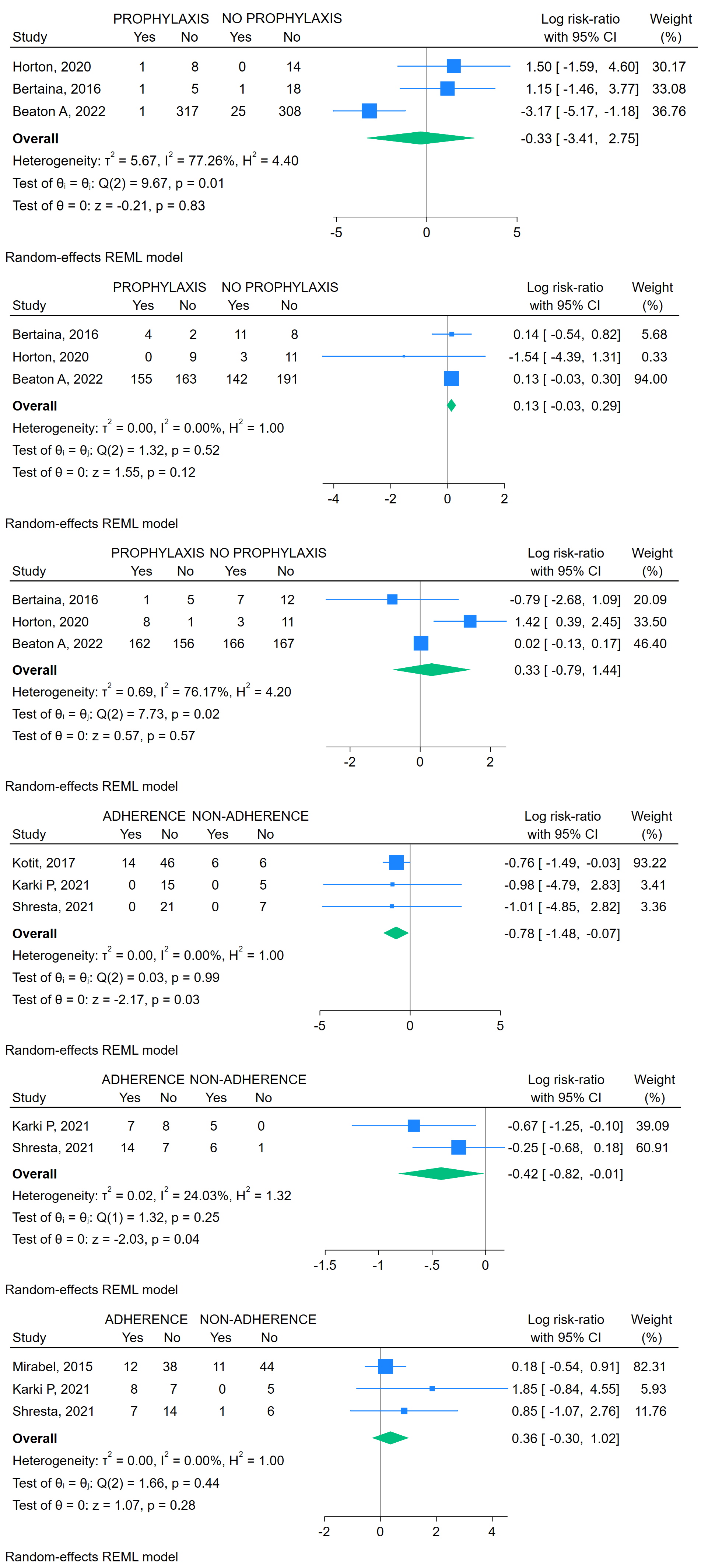
Prophylaxis vs. No Prophylaxis—Progression: log RR –0.33 (95 % CI –3.41 to 2.75), RR 0.72 (95 % CI 0.03–15.64; p=0.83; I2=77 %); Persistence: log RR 0.13 (95 % CI –0.03 to 0.29), RR 1.14 (95 % CI 0.97–1.34; p=0.12; I2=0 %); Regression: log RR 0.33 (95 % CI –0.79 to 1.44), RR 1.39 (95 % CI 0.45–4.22; p=0.57; I2=76 %).
Adherence vs. Non-Adherence—Progression: log RR –0.78 (95 % CI –1.48 to –0.07), RR 0.46 (95 % CI 0.23–0.93; p=0.03; I2=0 %); Persistence: log RR –0.42 (95 % CI –0.82 to –0.01), RR 0.66 (95 % CI 0.44–0.99; p=0.04; I2=24 %); Regression: log RR 0.36 (95 % CI –0.30 to 1.02), RR 1.43 (95 % CI 0.74–2.77; p=0.28; I2=0 %).
Conclusions
Penicillin prophylaxis alone did not significantly affect LRHD progression, persistence, or regression in our analysis, but high variability and bias may have affected these results. In contrast, prophylaxis adherence reduced progression by 54% (RR 0.46; p = 0.03) and persistence by 34% (RR 0.66; p = 0.04), while regression trended higher but was not significant. This highlights that prophylaxis appears to be effective only with proper medication adherence, which should be a priority for public policies aiming to reduce disease morbidity and mortality.
Background
Although Rheumatic Heart Disease prevalence has declined in high-income countries, it remains a major cause of morbidity and mortality in low-income areas. The 2012 WHF criteria define latent RHD (LRHD) as subclinical valvular lesions without classical RHD symptoms. LRHD may progress, persist, or regress, and the benefit of echocardiographic screening followed by penicillin prophylaxis remains unclear. For that reason, we developed a meta-analysis to investigate the effects of the penicillin prophylaxis, its adherence, and the outcomes on LRHD.
Hypothesis
Does penicillin prophylaxis reduce LRHD progression, persistence, or regression?
Does adherence affect these outcomes?
Methods
Following PRISMA and registered in PROSPERO (CRD420251012711), we searched PubMed, Embase, CENTRAL, and Scopus through February 18, 2025. Included studies compared prophylaxis versus no prophylaxis or adherent versus non-adherent LRHD patients (WHF 2012). Seven studies (n = 940; three RCTs, four cohorts) were included. Data extracted included event counts for progression, persistence, and regression. Risk of bias was assessed with RoB 2 and ROBINS-I. Random-effects REML models in Stata pooled log risk ratios (log RR) with 95 % CIs; heterogeneity was quantified by I2.
Results
Prophylaxis vs. No Prophylaxis—Progression: log RR –0.33 (95 % CI –3.41 to 2.75), RR 0.72 (95 % CI 0.03–15.64; p=0.83; I2=77 %); Persistence: log RR 0.13 (95 % CI –0.03 to 0.29), RR 1.14 (95 % CI 0.97–1.34; p=0.12; I2=0 %); Regression: log RR 0.33 (95 % CI –0.79 to 1.44), RR 1.39 (95 % CI 0.45–4.22; p=0.57; I2=76 %).
Adherence vs. Non-Adherence—Progression: log RR –0.78 (95 % CI –1.48 to –0.07), RR 0.46 (95 % CI 0.23–0.93; p=0.03; I2=0 %); Persistence: log RR –0.42 (95 % CI –0.82 to –0.01), RR 0.66 (95 % CI 0.44–0.99; p=0.04; I2=24 %); Regression: log RR 0.36 (95 % CI –0.30 to 1.02), RR 1.43 (95 % CI 0.74–2.77; p=0.28; I2=0 %).
Conclusions
Penicillin prophylaxis alone did not significantly affect LRHD progression, persistence, or regression in our analysis, but high variability and bias may have affected these results. In contrast, prophylaxis adherence reduced progression by 54% (RR 0.46; p = 0.03) and persistence by 34% (RR 0.66; p = 0.04), while regression trended higher but was not significant. This highlights that prophylaxis appears to be effective only with proper medication adherence, which should be a priority for public policies aiming to reduce disease morbidity and mortality.
More abstracts on this topic:
India as the Epicenter of Global Rheumatic Heart Disease: A Subnational and Temporal Analysis from 1990 to 2021
Patel Tirth, Sharma Kamal, Sethi Angad Singh, Gopi Gokul, Sharma Disha, Kotnani Sandeep, Upadhyay Devangi, Dudhat Kushal, Desai Hardik, Amin Vishrant
A Randomized Phase 2 Trial of Muvalaplin: An Oral Disrupter of the Assembly of Lipoprotein(a) ParticlesNicholls Stephen, Ni Wei, Rhodes Grace, Nissen Steven, Navar Ann Marie, Michael Laura, Krege John