Final ID: MP1215
Preliminary Results from the LiLAC Study: Living Life After Cardiogenic Shock Assessing Long-Term Quality of Life Outcomes Using Novel Digital Remote Monitoring Tools
Abstract Body (Do not enter title and authors here): Introduction: Studies on health-related quality of life (QoL) after discharge from cardiogenic shock (CS) are scarce. Patient-reported outcomes are essential to understanding long-term impacts of CS on daily functioning and resources for improving outcomes.
Hypothesis: We hypothesize that CS survivors experiencing worse functional limitations and psychological symptoms post-discharge and suffer higher readmission and mortality rates within 12 months.
Objective: LiLAC (Living Life After Cardiogenic Shock) is a prospective study quantifying the functional, psychological, and socioeconomic impairments experienced by CS survivors over 12 months post-discharge and how these metrics inform clinical outcomes.
Methods: LiLAC utilizes Eureka, a digital patient survey platform, to execute validated health-related QoL instruments including SF 20, MacArthur Ladder Scale, PROMIS, and GAD-7 completed at baseline, 1, 3, 6, and 12 months after discharge. Clinical data describing CS severity during admission are collected in REDCap, and multivariable regression and receiver operator curves are utilized to identify impactful disease features. [SHP1] [MOU2]
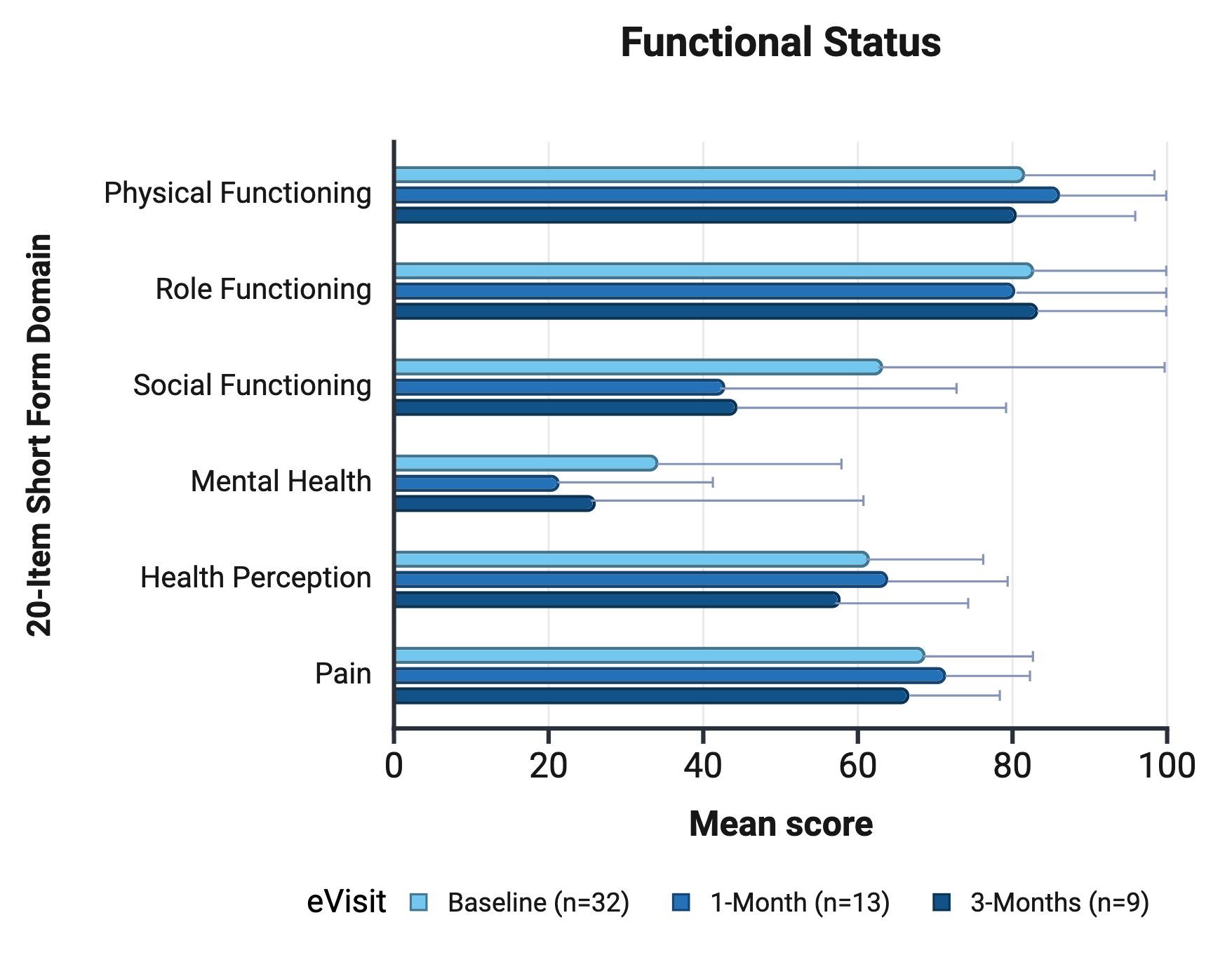
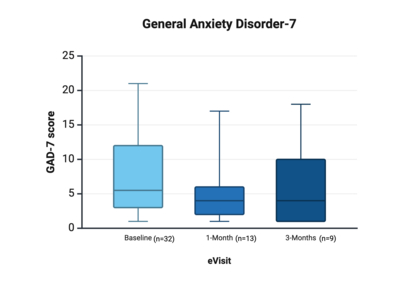
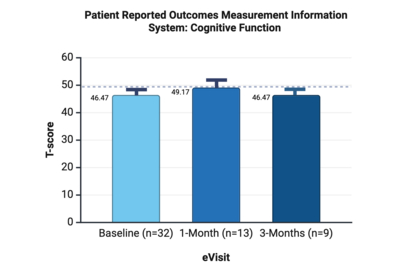
Results: Between December 9th, 2024, and May 7th, 2025, 96 [SHP3] patients were discharged from the Cardiac Intensive Care Unit after CS. 71 were eligible to participate. Of these, 46 (64%) [CO4] consented, with 32 (69%) completing baseline assessments, 13 (28%) completed the 1-month follow-up, and 9 (19%) completed the 3-month. GAD-7 scores improved from a median of 5.5 (IQR:3-12) at baseline to 4 (IQR:2-6) at 1 month. Cognitive function T-scores notably peaked at 49.2 at 1 month (PROMIS). Social functioning declined from 63.28 ± 39.14 at baseline to 42.86 ± 31.67 at 1 month and 44.44 ± 34.86 at 3 months (SF-20). Mental health scores were lowest at 1 month (21.43 ± 21.52). Seven participants self-reported heart-related readmissions at 1 month, and one at 3 months.
Conclusion: Early results demonstrate measurable impairments in functional status, psychological well-being, and cognitive function among CS survivors, . While readmission rates remain low, these data highlight the heterogeneity of post-discharge recovery underscoring the value of remote, standardized QoL monitoring. Low readmission and mortality events limit statistical analysis. Longitudinal associations between patient-reported outcomes and clinical events are prospectively being assessed and will be reported in full.
Hypothesis: We hypothesize that CS survivors experiencing worse functional limitations and psychological symptoms post-discharge and suffer higher readmission and mortality rates within 12 months.
Objective: LiLAC (Living Life After Cardiogenic Shock) is a prospective study quantifying the functional, psychological, and socioeconomic impairments experienced by CS survivors over 12 months post-discharge and how these metrics inform clinical outcomes.
Methods: LiLAC utilizes Eureka, a digital patient survey platform, to execute validated health-related QoL instruments including SF 20, MacArthur Ladder Scale, PROMIS, and GAD-7 completed at baseline, 1, 3, 6, and 12 months after discharge. Clinical data describing CS severity during admission are collected in REDCap, and multivariable regression and receiver operator curves are utilized to identify impactful disease features. [SHP1] [MOU2]
Results: Between December 9th, 2024, and May 7th, 2025, 96 [SHP3] patients were discharged from the Cardiac Intensive Care Unit after CS. 71 were eligible to participate. Of these, 46 (64%) [CO4] consented, with 32 (69%) completing baseline assessments, 13 (28%) completed the 1-month follow-up, and 9 (19%) completed the 3-month. GAD-7 scores improved from a median of 5.5 (IQR:3-12) at baseline to 4 (IQR:2-6) at 1 month. Cognitive function T-scores notably peaked at 49.2 at 1 month (PROMIS). Social functioning declined from 63.28 ± 39.14 at baseline to 42.86 ± 31.67 at 1 month and 44.44 ± 34.86 at 3 months (SF-20). Mental health scores were lowest at 1 month (21.43 ± 21.52). Seven participants self-reported heart-related readmissions at 1 month, and one at 3 months.
Conclusion: Early results demonstrate measurable impairments in functional status, psychological well-being, and cognitive function among CS survivors, . While readmission rates remain low, these data highlight the heterogeneity of post-discharge recovery underscoring the value of remote, standardized QoL monitoring. Low readmission and mortality events limit statistical analysis. Longitudinal associations between patient-reported outcomes and clinical events are prospectively being assessed and will be reported in full.
More abstracts on this topic:
Admission Cell-free DNA Predicts Cardiogenic Shock Progression and In-Hospital Mortality
Park Ashley, Kong Hyesik, Andargie Temesgen, Jang Moon, Solomon Michael, Brusca Samuel, Barnett Christopher, Obrien Connor, Agbor-enoh Sean
Assessing the Clinical Impact of Cardiac Intensivists in Cardiac Intensive Care Units.: Results from the RESCUE registryBae Dae-hwan, Bae Jang-whan, Lee Junyoung, Sun Jonghee, Lee Sang Yeub, Yang Jeong Hoon, Gwon Hyeon-cheol