Final ID: MP2250
Acute Myocardial Infarction and Stroke Outcomes Vary Substantially Across Private Equity Firms
Abstract Body (Do not enter title and authors here): Background: Private equity (PE) acquisitions of health care facilities have increased over the past decade, and growing evidence suggests this negatively affects patient outcomes. However, PE firms’ strategic priorities and operational approaches vary, raising the possibility that the effects on patient outcomes may differ across firms. Whether such heterogeneity exists remains unknown.
Research Question: We evaluated 30-day hospital revisits and 30-day mortality for acute myocardial infarction (AMI) and stroke at PE-acquired hospitals, and determined whether these outcomes differed across firms.
Methods: We identified US hospitals acquired by PE firms from 2013 to 2018. We compared the rates of 30-day revisits and 30-day mortality among Medicare fee-for-service beneficiaries aged 65 years and older with AMI or stroke between 2012 and 2019 at hospitals after PE acquisition. We excluded PE firms with less than 200 AMI or stroke hospitalizations. We then calculated median odds ratios (mOR) to quantify the variation in outcomes between PE firms. This represents the median increase in the odds of an outcome when an individual is switched from a with lower odds to a cluster with higher odds, holding all other factors constant.
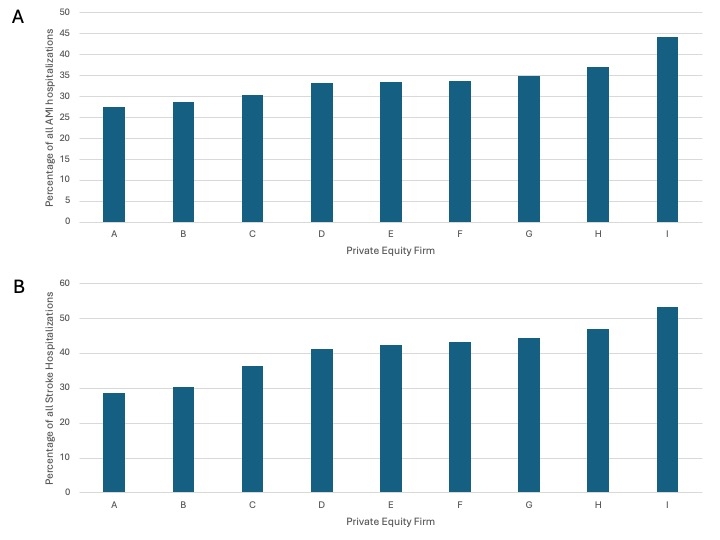
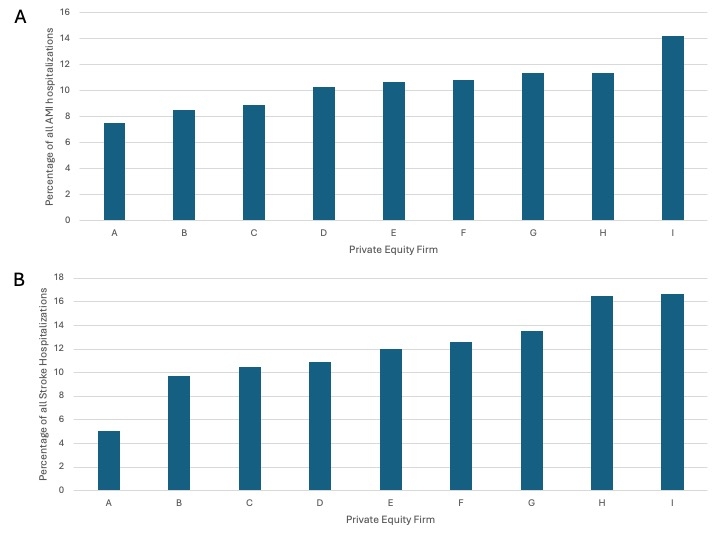
Results: We identified 40 PE-acquired hospitals that had Medicare data for AMI and stroke hospitalizations. There were 15 PE firm acquirers, 9 of which had more than 200 hospitalizations for AMI or stroke. The median AMI hospitalization rate across PE firms was 491 (IQR, 240-1105) and median stroke hospitalization rate was 530 (IQR, 223-914). Median 30-day revisit rate was 33.4% (IQR, 29.5%-36%) for AMI and 42.4% (IQR, 33.4%-45.6%) for stroke (Figure 1). Median 30-day mortality was 10.7% (IQR, 8.7%-11.4%) for AMI and 12.0% (IQR, 10.1%-15.0%) for stroke (Figure 2). After adjustment for age, sex, and clinical comorbidities, the mOR for 30-day revisits was 1.2 (CI, 1.09-1.35) for AMI and 1.28 (CI, 1.14-1.57) for stroke. In addition, the adjusted mOR for 30 day-mortality was 1.1 (CI, 1.00-1.93) for AMI and 1.17 (CI, 1.05-1.63) for stroke.
Conclusions: These findings reveal substantial variation in 30-day revisit and mortality rates for acute myocardial infarction and stroke among hospitals acquired by different PE firms. This heterogeneity underscores the need for further research to elucidate the strategic, operational, or structural factors that enable some PE firms to achieve better patient outcomes, while others fall short.
Research Question: We evaluated 30-day hospital revisits and 30-day mortality for acute myocardial infarction (AMI) and stroke at PE-acquired hospitals, and determined whether these outcomes differed across firms.
Methods: We identified US hospitals acquired by PE firms from 2013 to 2018. We compared the rates of 30-day revisits and 30-day mortality among Medicare fee-for-service beneficiaries aged 65 years and older with AMI or stroke between 2012 and 2019 at hospitals after PE acquisition. We excluded PE firms with less than 200 AMI or stroke hospitalizations. We then calculated median odds ratios (mOR) to quantify the variation in outcomes between PE firms. This represents the median increase in the odds of an outcome when an individual is switched from a with lower odds to a cluster with higher odds, holding all other factors constant.
Results: We identified 40 PE-acquired hospitals that had Medicare data for AMI and stroke hospitalizations. There were 15 PE firm acquirers, 9 of which had more than 200 hospitalizations for AMI or stroke. The median AMI hospitalization rate across PE firms was 491 (IQR, 240-1105) and median stroke hospitalization rate was 530 (IQR, 223-914). Median 30-day revisit rate was 33.4% (IQR, 29.5%-36%) for AMI and 42.4% (IQR, 33.4%-45.6%) for stroke (Figure 1). Median 30-day mortality was 10.7% (IQR, 8.7%-11.4%) for AMI and 12.0% (IQR, 10.1%-15.0%) for stroke (Figure 2). After adjustment for age, sex, and clinical comorbidities, the mOR for 30-day revisits was 1.2 (CI, 1.09-1.35) for AMI and 1.28 (CI, 1.14-1.57) for stroke. In addition, the adjusted mOR for 30 day-mortality was 1.1 (CI, 1.00-1.93) for AMI and 1.17 (CI, 1.05-1.63) for stroke.
Conclusions: These findings reveal substantial variation in 30-day revisit and mortality rates for acute myocardial infarction and stroke among hospitals acquired by different PE firms. This heterogeneity underscores the need for further research to elucidate the strategic, operational, or structural factors that enable some PE firms to achieve better patient outcomes, while others fall short.
More abstracts on this topic:
Advocacy in Cardiology: Healthcare lobbying and campaign finance activities of major cardiovascular professional societies, 2003 to 2023
Patel Prem, Milks Michael, Miller Andrew, Mehta Laxmi
A Stepwise Approach to Identifying and Assessing the Content Validity of Patient-Reported Outcome (PRO) Measures for Use with Adults with Acute Heart FailureO'connor Meaghan, Loughlin Anita, Waldman Laura, Rucker Sloan, Vaghela Shailja, Kwon Namhee, Sikirica Vanja