Final ID: MP1757
Impaired Peak VO2 at 3 Months Post-Acute Pulmonary Embolism is Independently Associated with Subsequent Development of Chronic Thromboembolic Pulmonary Hypertension
Abstract Body (Do not enter title and authors here): Introduction
Exercise limitation, commonly assessed by peak VO2, affects over 50% of acute pulmonary embolism (APE) survivors. Chronic thromboembolic pulmonary hypertension (CTEPH) is a rare but potentially fatal complication of APE. The association between post-APE exercise limitation and CTEPH development remains unclear.
Research Question
To determine the relationship between peak VO2 measured at 3 months post-APE and subsequent CTEPH, as well as pulmonary vascular disease (PVD) severity.
Methods
From a prospective registry of 846 consecutive hospitalized APE patients, we analyzed 319 individuals who underwent cardiopulmonary exercise testing at 3 months and had no prior pulmonary hypertension. Patients were stratified by peak VO2 tertiles. We used Kaplan-Meier analysis and Firth logistic regression to assess the relationship between peak VO2 and CTEPH. Patients who underwent right heart catheterization (RHC) during follow-up were re-stratified by peak VO2 tertiles to evaluate associations with PVD severity. Between-group comparisons were performed using ANOVA or Kruskal-Wallis tests.
Results
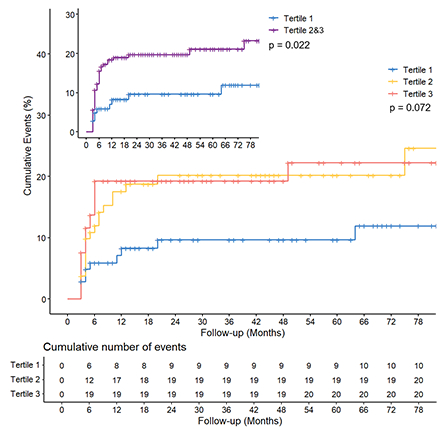
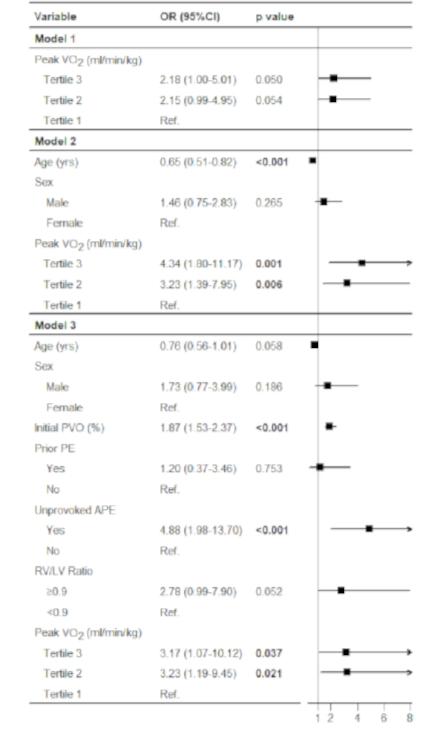
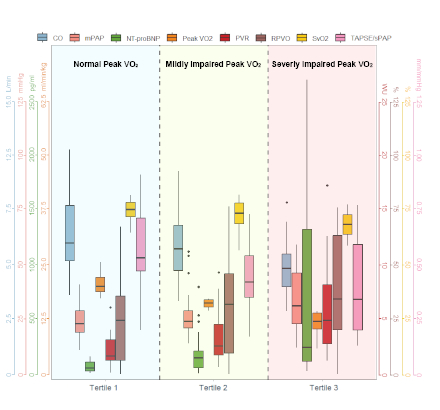
The cohort had a mean age of 60.8±13 years (45.8% male). Peak VO2 tertiles: tertile 1, >17.9 ml/min/kg; tertile 2, 14.3-17.9 ml/min/kg; tertile 3, <14.3 ml/min/kg. During a median follow-up of 36 months, 87 patients underwent RHC and 50 developed CTEPH. Cumulative CTEPH incidence was significantly lower in tertile 1 versus tertiles 2 and 3 combined (11.9% vs. 23.3%, log-rank p=0.022), but not among individual groups (11.9% vs. 24.6% vs. 22.2%, p=0.072). Tertiles 2 and 3 showed independent CTEPH associations (OR 3.23, 95% CI 1.19-9.45, p=0.021; OR 3.17, 95% CI 1.07-10.12, p=0.037). Among 87 catheterized patients, hemodynamic parameters demonstrated consistent deterioration across declining peak VO2 tertiles, with significant reductions in peak VO2, cardiac output, mixed venous oxygen saturation, and tricuspid annular plane systolic excursion to systolic pulmonary arterial pressure (PAP) ratio (p<0.001, p=0.001, p<0.001, and p=0.007, respectively), alongside increases in mean PAP, NT-proBNP, pulmonary vascular resistance, and residual pulmonary vascular obstruction (p=0.010, p<0.001, p<0.001, and p=0.055, respectively).
Conclusion
Impaired peak VO2 at 3 months post-APE independently associated with subsequent CTEPH and correlated with PVD severity, establishing peak VO2 as a valuable biomarker for early identification and management of post-APE PVD.
Exercise limitation, commonly assessed by peak VO2, affects over 50% of acute pulmonary embolism (APE) survivors. Chronic thromboembolic pulmonary hypertension (CTEPH) is a rare but potentially fatal complication of APE. The association between post-APE exercise limitation and CTEPH development remains unclear.
Research Question
To determine the relationship between peak VO2 measured at 3 months post-APE and subsequent CTEPH, as well as pulmonary vascular disease (PVD) severity.
Methods
From a prospective registry of 846 consecutive hospitalized APE patients, we analyzed 319 individuals who underwent cardiopulmonary exercise testing at 3 months and had no prior pulmonary hypertension. Patients were stratified by peak VO2 tertiles. We used Kaplan-Meier analysis and Firth logistic regression to assess the relationship between peak VO2 and CTEPH. Patients who underwent right heart catheterization (RHC) during follow-up were re-stratified by peak VO2 tertiles to evaluate associations with PVD severity. Between-group comparisons were performed using ANOVA or Kruskal-Wallis tests.
Results
The cohort had a mean age of 60.8±13 years (45.8% male). Peak VO2 tertiles: tertile 1, >17.9 ml/min/kg; tertile 2, 14.3-17.9 ml/min/kg; tertile 3, <14.3 ml/min/kg. During a median follow-up of 36 months, 87 patients underwent RHC and 50 developed CTEPH. Cumulative CTEPH incidence was significantly lower in tertile 1 versus tertiles 2 and 3 combined (11.9% vs. 23.3%, log-rank p=0.022), but not among individual groups (11.9% vs. 24.6% vs. 22.2%, p=0.072). Tertiles 2 and 3 showed independent CTEPH associations (OR 3.23, 95% CI 1.19-9.45, p=0.021; OR 3.17, 95% CI 1.07-10.12, p=0.037). Among 87 catheterized patients, hemodynamic parameters demonstrated consistent deterioration across declining peak VO2 tertiles, with significant reductions in peak VO2, cardiac output, mixed venous oxygen saturation, and tricuspid annular plane systolic excursion to systolic pulmonary arterial pressure (PAP) ratio (p<0.001, p=0.001, p<0.001, and p=0.007, respectively), alongside increases in mean PAP, NT-proBNP, pulmonary vascular resistance, and residual pulmonary vascular obstruction (p=0.010, p<0.001, p<0.001, and p=0.055, respectively).
Conclusion
Impaired peak VO2 at 3 months post-APE independently associated with subsequent CTEPH and correlated with PVD severity, establishing peak VO2 as a valuable biomarker for early identification and management of post-APE PVD.
More abstracts on this topic:
Can Stress Echocardiography during Cardiopulmonary Exercise Testing Help Predict Clinical Outcomes in Right-Sided Congenital Heart Disease?
Dizon Samantha, Krishnamurthy Yamini, Kochav Jonathan, Lewis Matthew, Rosenbaum Marlon, Zemer Wassercug Noa
Association of Moderate-Severe Tricuspid Regurgitation with Exercise Hemodynamics and Outcomes in Patients in Heart Failure with Preserved Ejection Fraction: Multicenter StudyDorsey Natalie, Caravita Sergio, Tedford Ryan, Rao Vishal N., Baratto Claudia, Biscopink Alec, Taylor Eric, Atkins Jessica, Amoroso Nicholas, Carnicelli Anthony, Houston Brian, Silkowski Molly