Final ID: MP473
Quality of Amiodarone Monitoring in a Veterans Affairs Healthcare System
Abstract Body (Do not enter title and authors here): Background: Amiodarone is widely utilized for managing atrial and ventricular arrhythmias, but is associated with pulmonary, liver, and thyroid toxicities. Previous studies demonstrated limited adherence to guidelines for amiodarone monitoring.
Research Question: To evaluate the quality of amiodarone monitoring and identify factors influencing its quality within the VA Greater Los Angeles Healthcare System (VAGLAHS).
Methods: This retrospective cohort study included Veterans ≥18 years with new amiodarone prescriptions between January 1, 2019 and July 31, 2023; hospice patients were excluded. Quality of monitoring outcomes included baseline pulmonary function tests (PFTs), chest X-ray (CXR), liver function tests (LFTs), thyroid function tests (TFTs; thyroid stimulating hormone (TSH) and free T4 (FT4)), and electrocardiogram (EKG), as well as LFTs and TSH at 6 months and 12 months after initiation. Logistic regression was used to identify characteristics associated with quality of monitoring, with potential variables chosen based on clinical judgment.
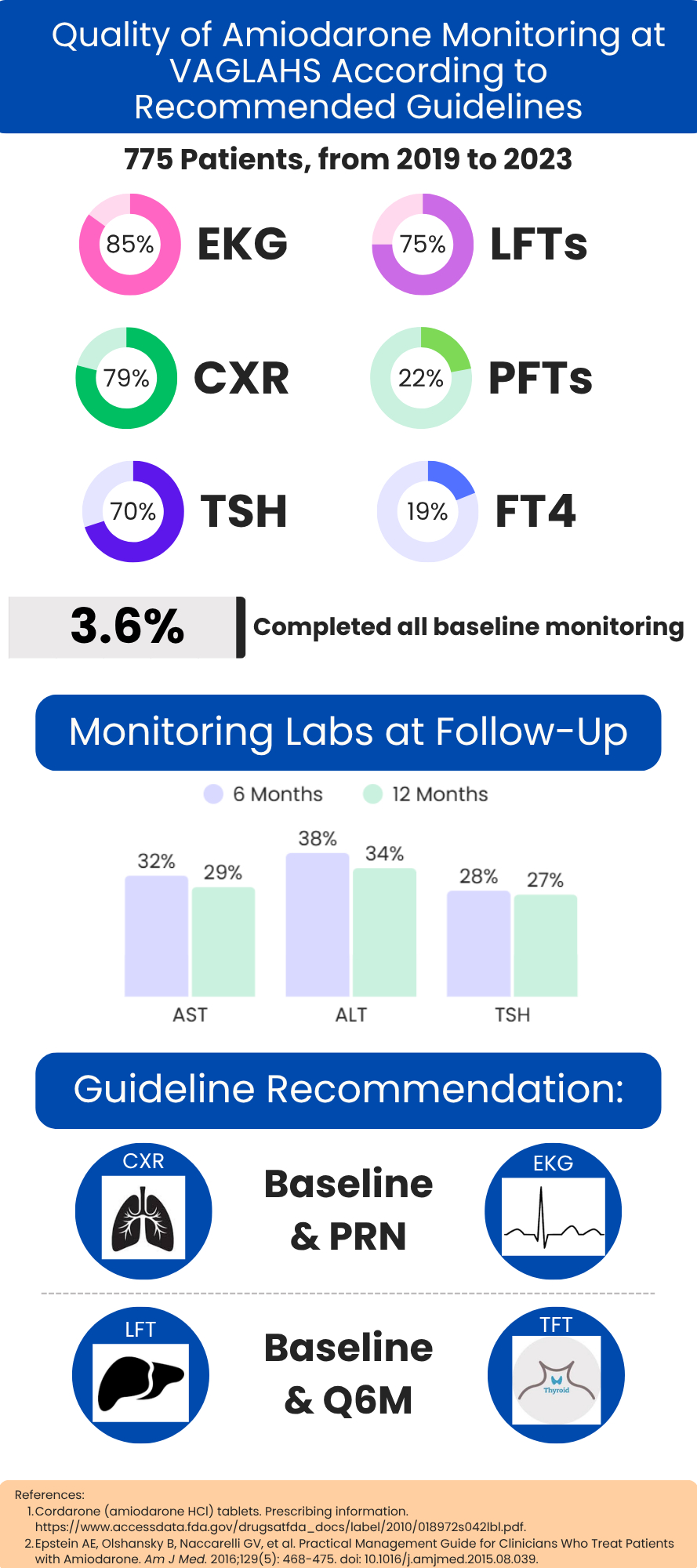
Results: Of 775 patients, 79% completed CXRs, 22% PFTs, 87% ALT, 75% AST, 70% TSH, 19% FT4, and 85% EKGs at baseline with 3.6% completing all baseline tests. Variables associated with baseline LFT monitoring included inpatient initiation (OR 3.30; 95%CI 2.21-4.93; P<0.0001), concomitant DOAC use (OR 2.65; 95%CI 1.79-3.93; P<0.0001), liver disease (OR 1.95; 95%CI 10.7-3.57; P=0.03), Black race (OR 1.61; 95%CI 1.00-2.56; P=0.05), age (OR 1.02; 95%CI 1.00-1.04; P=0.02) and VA initiation (OR 0.61; 95%CI 0.42-0.89; P=0.01). For baseline TFT monitoring, VA initiation was a positive factor (OR 1.60; 95%CI 1.07-2.40; P=0.02). At 6 months, 38%, 32%, and 28% had ALT, AST, and TSH evaluated respectively, with 34%, 29%, and 27% evaluated at 12 months. No medical visit at 6 or 12-months was associated with less LFT monitoring (6-month OR 0.09; 95%CI 0.03-0.28; P<0.0001, 12-months OR 0.16; 95%CI 0.05-0.51; P=0.002) and less TSH monitoring (6-months OR 0.13; 95%CI 0.04-0.40; P=0.0005, 12-months OR 0.21; 95%CI 0.06-0.77; P=0.02). A cardiology visit at 12 months (OR 2.32; 95%CI 1.25-4.31; P=0.008) was associated with TSH monitoring.
Conclusion: While a majority received CXR, LFTs and TSH monitoring at baseline, only a minority completed all baseline testing and monitoring was suboptimal at follow up. Future studies should investigate both reasons for lack of amiodarone monitoring and potential interventions for improvement.
Research Question: To evaluate the quality of amiodarone monitoring and identify factors influencing its quality within the VA Greater Los Angeles Healthcare System (VAGLAHS).
Methods: This retrospective cohort study included Veterans ≥18 years with new amiodarone prescriptions between January 1, 2019 and July 31, 2023; hospice patients were excluded. Quality of monitoring outcomes included baseline pulmonary function tests (PFTs), chest X-ray (CXR), liver function tests (LFTs), thyroid function tests (TFTs; thyroid stimulating hormone (TSH) and free T4 (FT4)), and electrocardiogram (EKG), as well as LFTs and TSH at 6 months and 12 months after initiation. Logistic regression was used to identify characteristics associated with quality of monitoring, with potential variables chosen based on clinical judgment.
Results: Of 775 patients, 79% completed CXRs, 22% PFTs, 87% ALT, 75% AST, 70% TSH, 19% FT4, and 85% EKGs at baseline with 3.6% completing all baseline tests. Variables associated with baseline LFT monitoring included inpatient initiation (OR 3.30; 95%CI 2.21-4.93; P<0.0001), concomitant DOAC use (OR 2.65; 95%CI 1.79-3.93; P<0.0001), liver disease (OR 1.95; 95%CI 10.7-3.57; P=0.03), Black race (OR 1.61; 95%CI 1.00-2.56; P=0.05), age (OR 1.02; 95%CI 1.00-1.04; P=0.02) and VA initiation (OR 0.61; 95%CI 0.42-0.89; P=0.01). For baseline TFT monitoring, VA initiation was a positive factor (OR 1.60; 95%CI 1.07-2.40; P=0.02). At 6 months, 38%, 32%, and 28% had ALT, AST, and TSH evaluated respectively, with 34%, 29%, and 27% evaluated at 12 months. No medical visit at 6 or 12-months was associated with less LFT monitoring (6-month OR 0.09; 95%CI 0.03-0.28; P<0.0001, 12-months OR 0.16; 95%CI 0.05-0.51; P=0.002) and less TSH monitoring (6-months OR 0.13; 95%CI 0.04-0.40; P=0.0005, 12-months OR 0.21; 95%CI 0.06-0.77; P=0.02). A cardiology visit at 12 months (OR 2.32; 95%CI 1.25-4.31; P=0.008) was associated with TSH monitoring.
Conclusion: While a majority received CXR, LFTs and TSH monitoring at baseline, only a minority completed all baseline testing and monitoring was suboptimal at follow up. Future studies should investigate both reasons for lack of amiodarone monitoring and potential interventions for improvement.
More abstracts on this topic:
Characterization of Novel Cardiovascular Medication Use by Clinical Specialty After Admission for Heart Failure or Coronary Artery Disease
Salahuddin Taufiq, Chow Christine, Hebbe Annika, Simons Carol, Helfrich Christian, Doll Jacob
1-year comparison of quadruple therapy sequencing strategies for heart failure with reduced ejection fraction using an individual-based state-transition microsimulation modelTurgeon Ricky, Van Minh Tri, Loewen Peter, Hawkins Nathaniel, Sadatsafavi Mohsen, Zhang Wei, Mackay Kelly