Final ID: MP2546
Predictive utility of effective regurgitation orifice area to left ventricular end diastolic volume ratio in MitraClip treatment: Outcomes from a multi-center study.
Abstract Body (Do not enter title and authors here): Introduction
MitraClip (MC) placement for transcatheter edge-to-edge repair (TEER) is being increasingly utilized for treatment of secondary mitral regurgitation (SMR). The aim of this study was to analyze one-year outcomes after MC placement as well as the utility of pre-procedural EROA/LVEDV (effective regurgitation orifice area/left ventricular end diastolic volume) ratio in predicting outcomes.
Methods
We analyzed patients who underwent MitraClip placement at three centers. Primary efficacy endpoint (PEE) was determined by absence of heart failure (HF) hospitalizations at one year follow up. One way ANOVA was used to determine variance of pre-procedural EROA/LVEDV ratio between the outcome groups. Multivariate regression analysis was done to identify pre-procedural echocardiographic parameters that held significant association with symptom improvement. ROC analysis was done between the ratio and symptom improvement. A two tailed p-value < 0.05 was used to determine statistical significance.
Results
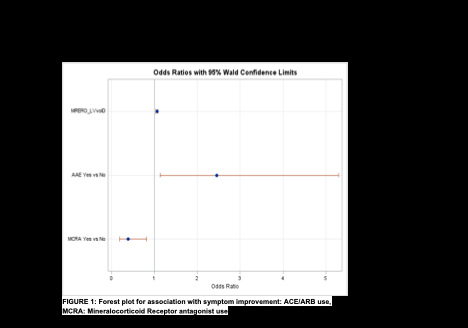
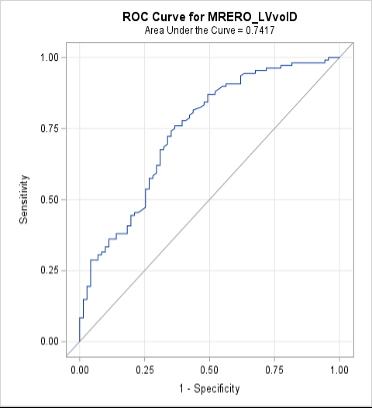
Between January of 2021 and March 2024, 236 patients underwent MitraClip placement, of which 157 patients (66.52%) reached PEE. Mean effective regurgitant orifice area (EROA) was 0.38 cm2 (0.32 - 0.44) in the symptom worsening group, compared to 0.52 cm2 (0.43 - 0.61) in patients that reached PEE. The mean left ventricular end diastolic volume (LVEDV) in the symptom worsening group was 110.58 mL (95.83 - 125.32) compared to 74.56 mL (62.55 - 86.57) in the patients that reached PEE. A ratio between EROA and LVEDV (EROA/ LVEDV x 100) was measured to quantify disproportionate secondary mitral regurgitation (SMR). After multivariate regression analysis, the ratio was found to have a significant association with symptom improvement (OR: 1.059 (1.032 –1.087, p value < 0.001). Forest plots depicted in Figure 1. ROC curve analysis had an area under the curve (AUC) of 0.7417 (0.669- 0.816) making it a better predictor for symptom improvement (Figure 2). Youden Index was calculated at 0.184 with 87% sensitivity and 51.4% specificity (Index: 0.39048).
Conclusions
After regressing for confounding factors, a preprocedural EROA/ LVEDV ratio (EROA/LVEDV x 100) > 0.184 had 87% sensitivity in predicting symptom improvement. The ratio had significant association with symptom improvement group after multivariate regression analysis.
MitraClip (MC) placement for transcatheter edge-to-edge repair (TEER) is being increasingly utilized for treatment of secondary mitral regurgitation (SMR). The aim of this study was to analyze one-year outcomes after MC placement as well as the utility of pre-procedural EROA/LVEDV (effective regurgitation orifice area/left ventricular end diastolic volume) ratio in predicting outcomes.
Methods
We analyzed patients who underwent MitraClip placement at three centers. Primary efficacy endpoint (PEE) was determined by absence of heart failure (HF) hospitalizations at one year follow up. One way ANOVA was used to determine variance of pre-procedural EROA/LVEDV ratio between the outcome groups. Multivariate regression analysis was done to identify pre-procedural echocardiographic parameters that held significant association with symptom improvement. ROC analysis was done between the ratio and symptom improvement. A two tailed p-value < 0.05 was used to determine statistical significance.
Results
Between January of 2021 and March 2024, 236 patients underwent MitraClip placement, of which 157 patients (66.52%) reached PEE. Mean effective regurgitant orifice area (EROA) was 0.38 cm2 (0.32 - 0.44) in the symptom worsening group, compared to 0.52 cm2 (0.43 - 0.61) in patients that reached PEE. The mean left ventricular end diastolic volume (LVEDV) in the symptom worsening group was 110.58 mL (95.83 - 125.32) compared to 74.56 mL (62.55 - 86.57) in the patients that reached PEE. A ratio between EROA and LVEDV (EROA/ LVEDV x 100) was measured to quantify disproportionate secondary mitral regurgitation (SMR). After multivariate regression analysis, the ratio was found to have a significant association with symptom improvement (OR: 1.059 (1.032 –1.087, p value < 0.001). Forest plots depicted in Figure 1. ROC curve analysis had an area under the curve (AUC) of 0.7417 (0.669- 0.816) making it a better predictor for symptom improvement (Figure 2). Youden Index was calculated at 0.184 with 87% sensitivity and 51.4% specificity (Index: 0.39048).
Conclusions
After regressing for confounding factors, a preprocedural EROA/ LVEDV ratio (EROA/LVEDV x 100) > 0.184 had 87% sensitivity in predicting symptom improvement. The ratio had significant association with symptom improvement group after multivariate regression analysis.
More abstracts on this topic:
A Comparison of Anxiety and Depression in Patients with Symptoms of Palpitations Compared to High Risk Arrythmia Patients.
Treuth Mark, Patel Kunnal, Rissmiller Justin, Holdai Veera
A Rare Case of Epicardial Cavernous Hemangioma with Coexisting Severe Mitral RegurgitationAbdallah Ala, Sutton Jenna, Houshmand Nazanin, Gupta Neelesh, Ahsan Chowdhury