Final ID: MP769
Ventricular Tachycardia Ablation in Patients with and Without Chronic Kidney Disease
Abstract Body (Do not enter title and authors here): Background: Chronic kidney disease (CKD) is a commonly coexisting condition in patients undergoing ventricular tachycardia (VT) ablation and may be associated with worse procedural and long-term outcomes. Patients with CKD often have a higher burden of structural heart disease, inflammation, and arrhythmogenic substrate, which may contribute to adverse post-ablation outcomes. Despite this, limited real-world data exist evaluating the impact of CKD on long-term clinical outcomes following VT ablation. We sought to evaluate the association between CKD and post-procedural outcomes in patients undergoing VT ablation using a large multicenter database.
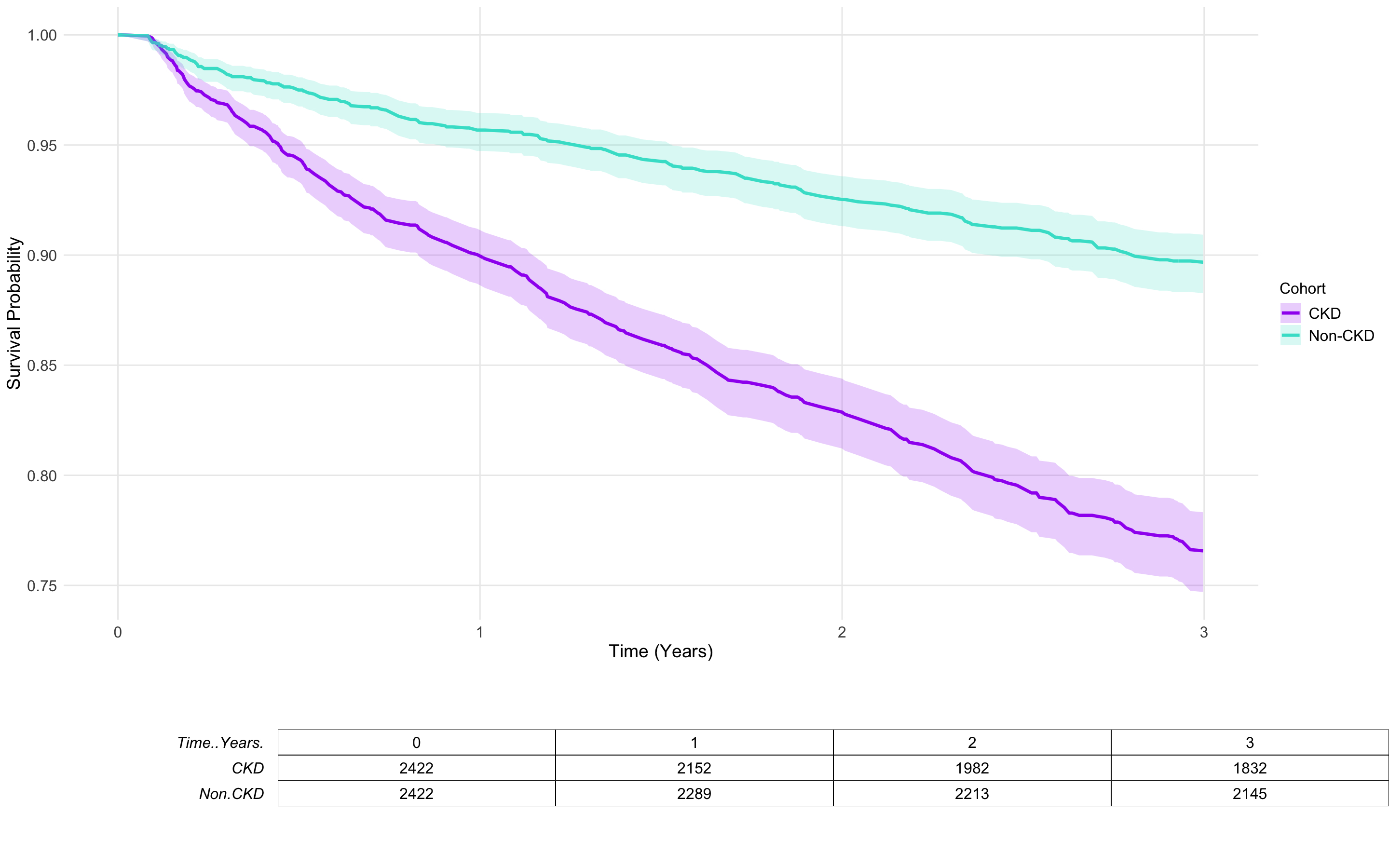
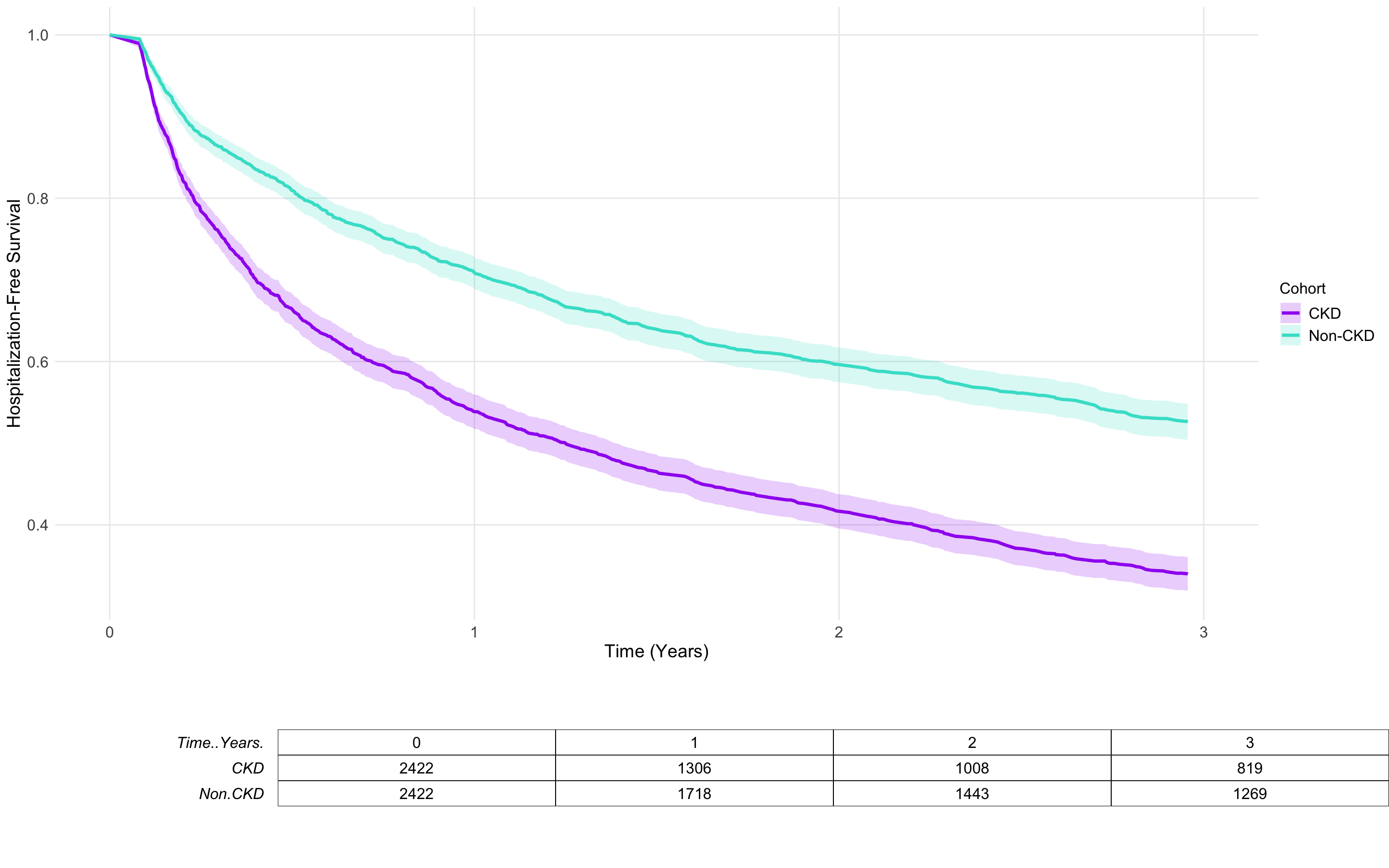
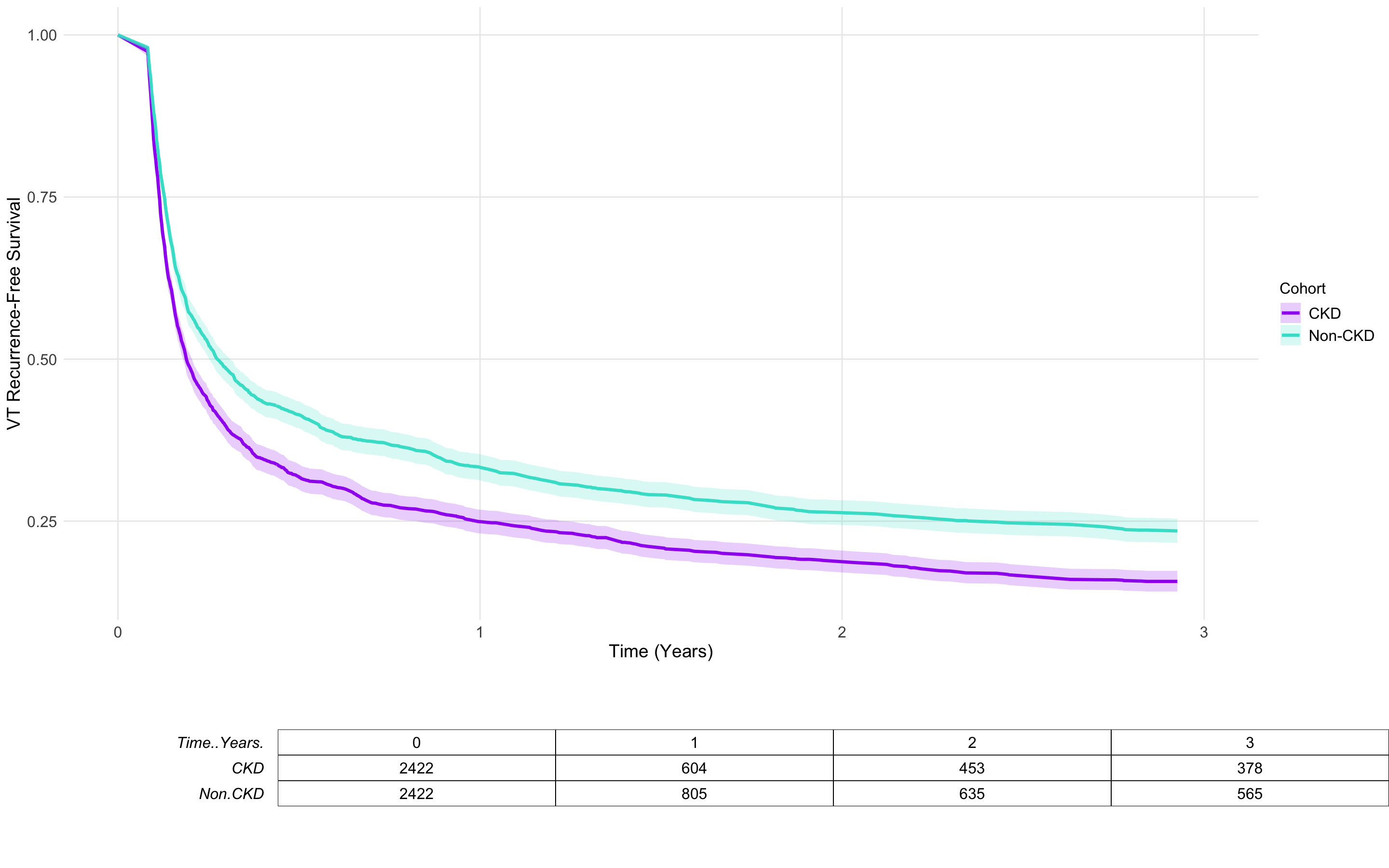
Methods: Using TriNetX research network dataset, we identified 10,009 adult (≥18 years) patients who underwent catheter ablation for VT from January 2015 to December 2021. For our analyses, we stratified patients into two cohorts: those with CKD and those without CKD. Propensity score matching (1:1) was performed to balance demographics, comorbidities, and medications, resulting in 2,422 matched patients per group. Patients were followed for up to 3 years after the index ablation procedure.The primary outcome was all-cause mortality. Secondary outcomes included hospitalization and VT recurrence. Kaplan-Meier analysis and Cox proportional hazards models were used to estimate hazard ratios (HRs) for the comparison of these clinical outcomes.
Results: Over the 3-year follow-up period, patients in the CKD group had significantly higher all-cause mortality compared to the non-CKD group (20.6% vs. 8.7%; HR: 2.45, 95% CI: 2.08–2.88; p < 0.0001). CKD patients were also more likely to be hospitalized following VT ablation (58.2% vs. 40.0%; HR: 1.72, 95% CI: 1.58–1.87; p < 0.0001). Additionally, VT recurrence was significantly more common in the CKD group compared to those without CKD (76.6% vs. 67.8%; HR: 1.28, 95% CI: 1.20–1.37; p < 0.0001).
Conclusions: In patients undergoing VT ablation, CKD was independently associated with significantly increased risks of mortality, hospitalization, and VT recurrence. These findings highlight the importance of incorporating CKD as an independent risk factor for poorer clinical outcomes after VT ablation. Enhanced risk stratification and tailored peri-procedural management may be warranted in this high-risk population to improve outcomes.
Methods: Using TriNetX research network dataset, we identified 10,009 adult (≥18 years) patients who underwent catheter ablation for VT from January 2015 to December 2021. For our analyses, we stratified patients into two cohorts: those with CKD and those without CKD. Propensity score matching (1:1) was performed to balance demographics, comorbidities, and medications, resulting in 2,422 matched patients per group. Patients were followed for up to 3 years after the index ablation procedure.The primary outcome was all-cause mortality. Secondary outcomes included hospitalization and VT recurrence. Kaplan-Meier analysis and Cox proportional hazards models were used to estimate hazard ratios (HRs) for the comparison of these clinical outcomes.
Results: Over the 3-year follow-up period, patients in the CKD group had significantly higher all-cause mortality compared to the non-CKD group (20.6% vs. 8.7%; HR: 2.45, 95% CI: 2.08–2.88; p < 0.0001). CKD patients were also more likely to be hospitalized following VT ablation (58.2% vs. 40.0%; HR: 1.72, 95% CI: 1.58–1.87; p < 0.0001). Additionally, VT recurrence was significantly more common in the CKD group compared to those without CKD (76.6% vs. 67.8%; HR: 1.28, 95% CI: 1.20–1.37; p < 0.0001).
Conclusions: In patients undergoing VT ablation, CKD was independently associated with significantly increased risks of mortality, hospitalization, and VT recurrence. These findings highlight the importance of incorporating CKD as an independent risk factor for poorer clinical outcomes after VT ablation. Enhanced risk stratification and tailored peri-procedural management may be warranted in this high-risk population to improve outcomes.
More abstracts on this topic:
Artificial Intelligence ECG Analysis More Accurately Identifies Epicardial versus Endocardial Ventricular Tachycardia and Pacing Compared with Visual Criteria
Dreessens Erin, Feld Gregory, Mcculloch Andrew, Villongco Christopher, Ho Gordon, Krummen David, Oliver Kendall, Fox Sutton, Sung Kevin, Aldaas Omar, Han Frederick, Hoffmayer Kurt, Hsu Jonathan, Raissi Farshad
A Refractory Case of Prinzmetal’s Angina Treated with VATS SympathectomyQureshi Natasha, Vashistha Kirtivardhan, Ali Syed, Omar Ali, Kanei Yumiko