Final ID: MP2091
Last-Resort Rotational Atherectomy for Balloon-Uncrossable Calcified SVG to OM Graft: A Case Report
Abstract Body (Do not enter title and authors here): Heavily calcified SVG lesions are rare and challenging, with limited evidence supporting atherectomy during PCI.
Case: A 75-year-old female with CAD, prior CABG, AFib, and ESRD presented with worsening angina. Angiography showed patent LIMA-LAD, occluded SVG-RCA, severely diseased SVG-OM, and significant LCX disease. RCA PCI was done. LCX was unsuitable for PCI due to tortuosity and tandem CTOs. SVG-OM PCI failed due to balloon uncrossability. Medical therapy was initiated, but ischemia persisted in the lateral wall despite triple anti-anginal therapy.
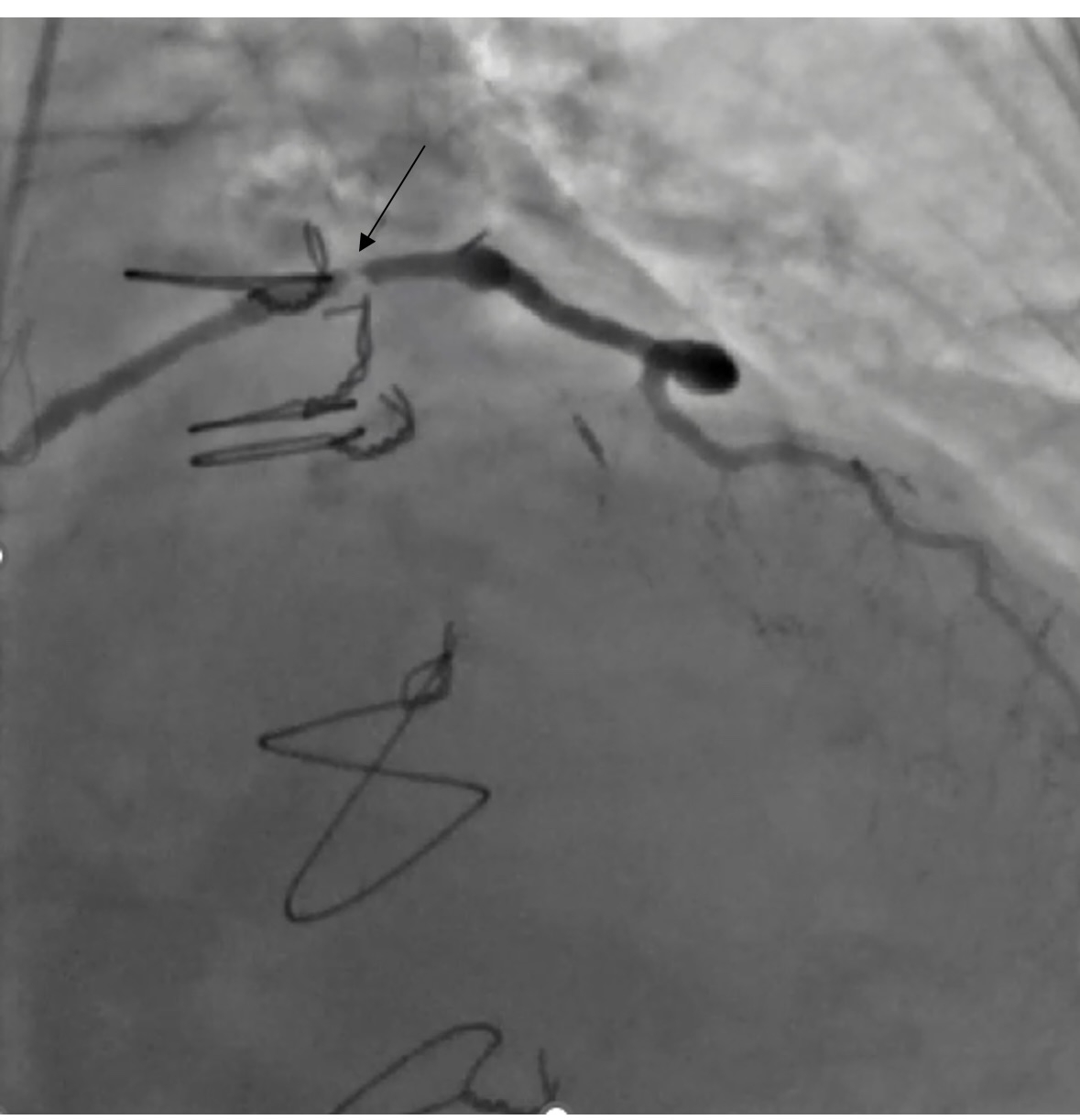
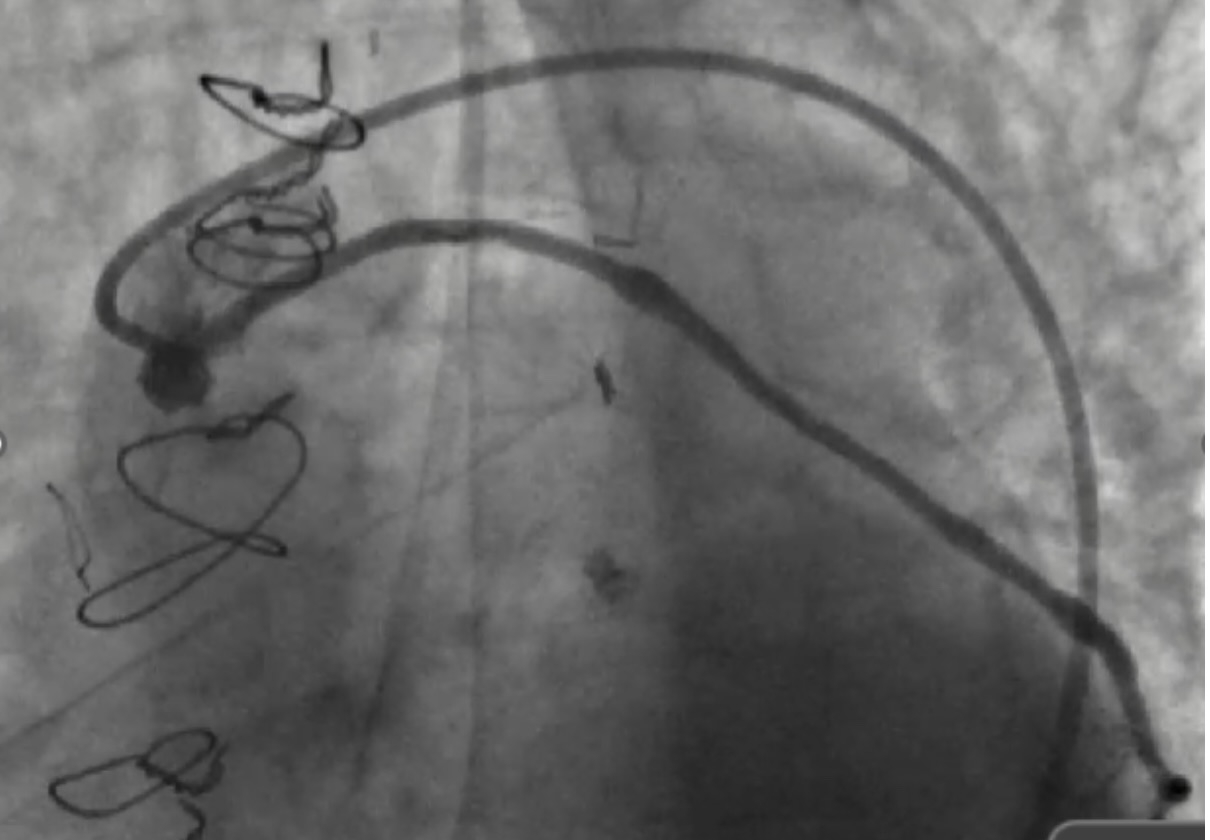
After shared decision-making, high-risk PCI was pursued. We used 7F equipment and an AL 0.75 guide. Angiography confirmed a severely calcified mid and ostial SVG lesion. A workhorse wire crossed the lesion, but neither microcatheter nor balloon could be advanced. These lesion characteristics even made Embolic protection devices (EPDs) infeasible and hence were not used. Laser Atherectomy was avoided due to heavy calcification, and Intravascular lithotripsy (IVL) was not feasible due to its large profile. Rotational atherectomy was pursued as a last resort. A microcatheter was deeply positioned, and a Rota floppy wire was advanced using a primary wiring technique. We then performed rotational atherectomy in the SVG graft with a 1.25 mm burr at 150,000 rpm. No perforation or vessel damage was seen. Subsequently sequential balloon angioplasty and stenting with 2.75 x 38 and 2.75 x26 mm stents were placed from distal graft body to ostium with significantly improved blood flow in the graft. Bailout strategies, including vascular plugs, coils, covered stents, and vasodilators, were prepared, alongside plans for prolonged DAPT.
Discussion: SVG calcification involves the vessel wall, leading to diffuse disease and higher PCI risks due to small distal vessels, recoil, and disease beyond the graft. Atherectomy is usually avoided in SVGs due to limited data and risks like embolization, perforation, no-reflow, and MACE. It is recommended to use EPDs to reduce the risk of distal embolization, no-reflow, and periprocedural MI. Vasodilators, direct stenting, and undersized stents may help mitigate no-reflow and distal embolization. In this case, technical limitations, extreme calcification and failure to cross the lesion with standard devices necessitated rotational atherectomy. This case supports the selective use of rotational atherectomy in complex SVG lesions and emphasizes the need for further study to guide management.
Case: A 75-year-old female with CAD, prior CABG, AFib, and ESRD presented with worsening angina. Angiography showed patent LIMA-LAD, occluded SVG-RCA, severely diseased SVG-OM, and significant LCX disease. RCA PCI was done. LCX was unsuitable for PCI due to tortuosity and tandem CTOs. SVG-OM PCI failed due to balloon uncrossability. Medical therapy was initiated, but ischemia persisted in the lateral wall despite triple anti-anginal therapy.
After shared decision-making, high-risk PCI was pursued. We used 7F equipment and an AL 0.75 guide. Angiography confirmed a severely calcified mid and ostial SVG lesion. A workhorse wire crossed the lesion, but neither microcatheter nor balloon could be advanced. These lesion characteristics even made Embolic protection devices (EPDs) infeasible and hence were not used. Laser Atherectomy was avoided due to heavy calcification, and Intravascular lithotripsy (IVL) was not feasible due to its large profile. Rotational atherectomy was pursued as a last resort. A microcatheter was deeply positioned, and a Rota floppy wire was advanced using a primary wiring technique. We then performed rotational atherectomy in the SVG graft with a 1.25 mm burr at 150,000 rpm. No perforation or vessel damage was seen. Subsequently sequential balloon angioplasty and stenting with 2.75 x 38 and 2.75 x26 mm stents were placed from distal graft body to ostium with significantly improved blood flow in the graft. Bailout strategies, including vascular plugs, coils, covered stents, and vasodilators, were prepared, alongside plans for prolonged DAPT.
Discussion: SVG calcification involves the vessel wall, leading to diffuse disease and higher PCI risks due to small distal vessels, recoil, and disease beyond the graft. Atherectomy is usually avoided in SVGs due to limited data and risks like embolization, perforation, no-reflow, and MACE. It is recommended to use EPDs to reduce the risk of distal embolization, no-reflow, and periprocedural MI. Vasodilators, direct stenting, and undersized stents may help mitigate no-reflow and distal embolization. In this case, technical limitations, extreme calcification and failure to cross the lesion with standard devices necessitated rotational atherectomy. This case supports the selective use of rotational atherectomy in complex SVG lesions and emphasizes the need for further study to guide management.
More abstracts on this topic:
Safety and Efficacy of Radial Versus Femoral Access for Rotational Atherectomy: An Updated Systematic Review And Meta-Analysis
Ahmed Muhammad, Murtaza Muzna, Muzammil Muhammad, Sami Syeda Zuha, Nazir Ariba, Ahmed Muhammad, Asghar Muhammad Sohaib
Innovative Use Of Rotational Atherectomy In Heavily Calcified Superior Mesenteric Artery StenosisKazmi Farwa, Jehangir Qasim, Gjeka Rudin