Final ID: MP2203
Relations Of Inflammatory Biomarkers With Incident Clinical Peripheral Artery Disease In Older Adults
Abstract Body (Do not enter title and authors here): Background
Peripheral artery disease (PAD) is a vascular condition marked by arterial narrowing that affects 8.5 million adults in the U.S. Contributions of circulating biomarkers reflecting different immune pathways have not been well established in large population-based studies of older adults.
Hypothesis
We hypothesized that nine inflammatory biomarkers would be associated with increased risk of incident clinical PAD and incident low ankle-brachial index (ABI), independent of risk factors.
Methods
We used available data from 5888 adults ≥65 years enrolled in the Cardiovascular Health Study. Nine inflammatory biomarkers measured at baseline were evaluated: soluble CD14 (sCD14), interleukin-6 (IL-6), high sensitivity C-reactive protein (hsCRP), white blood cell count (WBC), soluble CD163 (sCD163), interleukin-18 (IL-18), interleukin-1 receptor antagonist (IL-1RA), soluble tumor necrosis factor receptor 1 (sTNFR1), and soluble interleukin-2 receptor alpha (sIL2Rα). Clinical PAD was defined as exertional lower extremity discomfort relieved by rest, imaging evidence, revascularization procedure, or claudication. ABI was assessed in 1989-90 in the first CHS cohort of predominantly white participants, or in 1992-93 for the second CHS cohort of predominantly black participants (baseline), and again in 1998-99 (follow-up). Incident low ABI was defined as a >0.15 drop in ABI and follow-up ABI<0.9. Cox regression was used for incident PAD, and Poisson regression for incident low ABI. Model adjusted for demographic, behavioral, and clinical risk factors.
Results
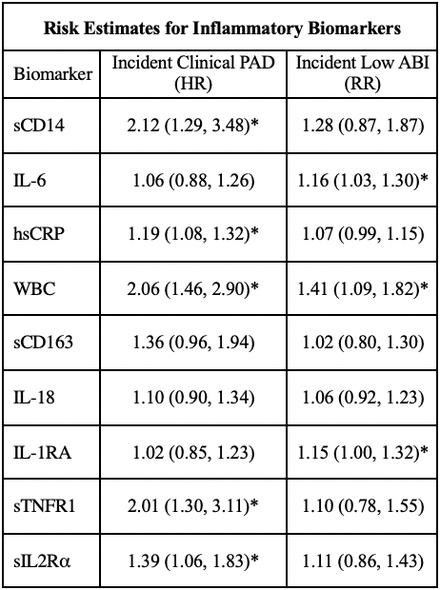
After excluding participants with prevalent PAD or ABI<0.9 at baseline, 5061 (41% men, 85% white) were included for the incident clinical PAD analysis. Over a median follow-up of 13.9 years, 260 participants developed clinical PAD. For incident low ABI, further exclusions for ABI>1.4 or missing follow-up ABI yielded 2435 participants for analysis, of which 359 had incident low ABI over a median interval of 8 years. Five biomarkers, sCD14, hsCRP, WBC, sTNFR1, and sIL2Rα, were associated with incident PAD. While three biomarkers, IL-6, WBC, and IL-1RA, were associated with incident low ABI.
Conclusions
Several markers of inflammation, monocyte stimulation, and adaptive immune activation were associated with incident PAD, while those signaling general inflammation and NLRP3 activation were associated with incident low ABI. Additional work will identify specific inflammatory pathways as targets for PAD in elders.
Peripheral artery disease (PAD) is a vascular condition marked by arterial narrowing that affects 8.5 million adults in the U.S. Contributions of circulating biomarkers reflecting different immune pathways have not been well established in large population-based studies of older adults.
Hypothesis
We hypothesized that nine inflammatory biomarkers would be associated with increased risk of incident clinical PAD and incident low ankle-brachial index (ABI), independent of risk factors.
Methods
We used available data from 5888 adults ≥65 years enrolled in the Cardiovascular Health Study. Nine inflammatory biomarkers measured at baseline were evaluated: soluble CD14 (sCD14), interleukin-6 (IL-6), high sensitivity C-reactive protein (hsCRP), white blood cell count (WBC), soluble CD163 (sCD163), interleukin-18 (IL-18), interleukin-1 receptor antagonist (IL-1RA), soluble tumor necrosis factor receptor 1 (sTNFR1), and soluble interleukin-2 receptor alpha (sIL2Rα). Clinical PAD was defined as exertional lower extremity discomfort relieved by rest, imaging evidence, revascularization procedure, or claudication. ABI was assessed in 1989-90 in the first CHS cohort of predominantly white participants, or in 1992-93 for the second CHS cohort of predominantly black participants (baseline), and again in 1998-99 (follow-up). Incident low ABI was defined as a >0.15 drop in ABI and follow-up ABI<0.9. Cox regression was used for incident PAD, and Poisson regression for incident low ABI. Model adjusted for demographic, behavioral, and clinical risk factors.
Results
After excluding participants with prevalent PAD or ABI<0.9 at baseline, 5061 (41% men, 85% white) were included for the incident clinical PAD analysis. Over a median follow-up of 13.9 years, 260 participants developed clinical PAD. For incident low ABI, further exclusions for ABI>1.4 or missing follow-up ABI yielded 2435 participants for analysis, of which 359 had incident low ABI over a median interval of 8 years. Five biomarkers, sCD14, hsCRP, WBC, sTNFR1, and sIL2Rα, were associated with incident PAD. While three biomarkers, IL-6, WBC, and IL-1RA, were associated with incident low ABI.
Conclusions
Several markers of inflammation, monocyte stimulation, and adaptive immune activation were associated with incident PAD, while those signaling general inflammation and NLRP3 activation were associated with incident low ABI. Additional work will identify specific inflammatory pathways as targets for PAD in elders.
More abstracts on this topic:
Association Between Blood Pressure and Clinical Events in Peripheral Artery Disease with Small Vessel Disease
Nathani Rohit, Girotra Saket, Vaughan Sarrazin Mary, Chan Paul, Gupta Ajay, Kumbhani Dharam, Li Qiang, Nguyen Cathy, De Lemos James, Beckman Joshua
A Shocking Development After Peripheral Arterial InterventionAggarwal Devika, Badar Mustanser, Gowda Ramesh