Final ID: MP1889
Short-term Particulate Matter 2.5 Exposure and Chronic Psychosocial Stress Cause Maladaptive Remodeling in the Heart.
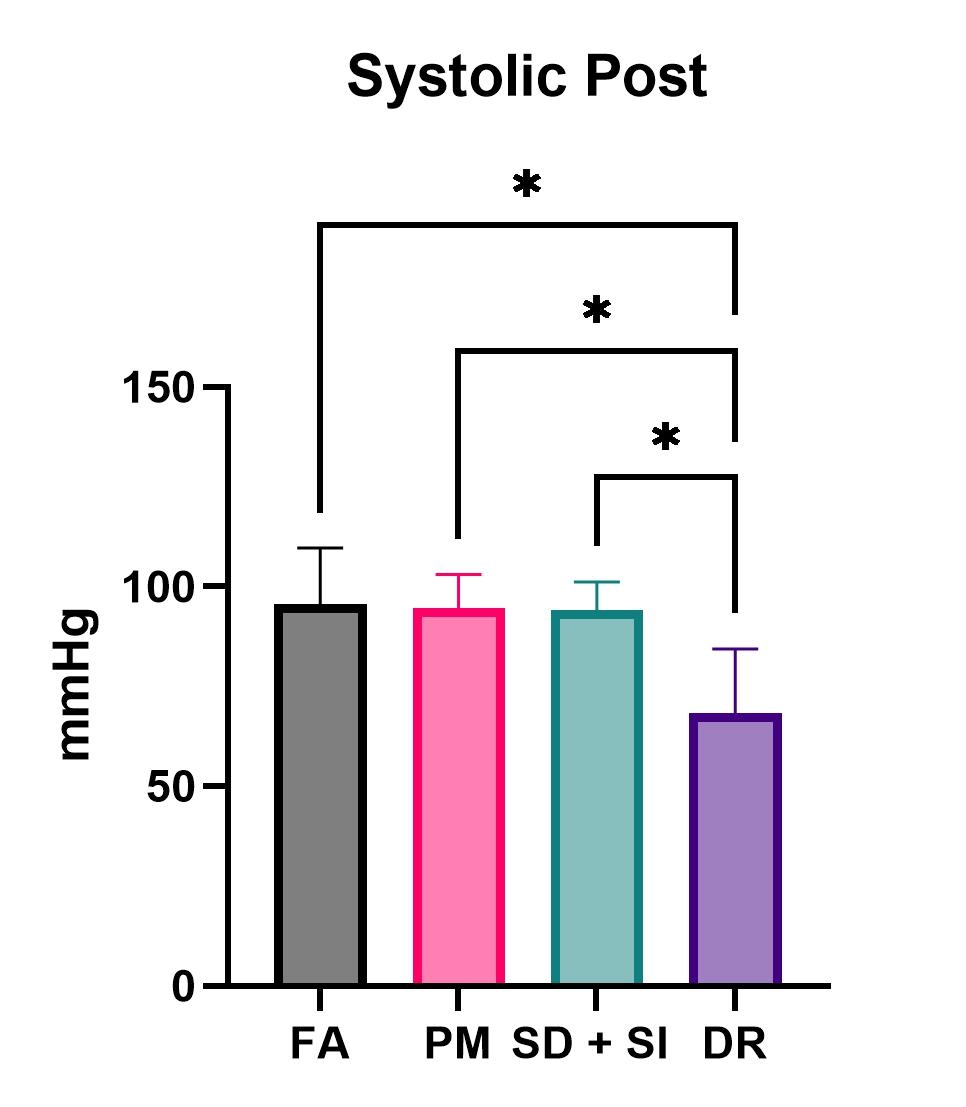
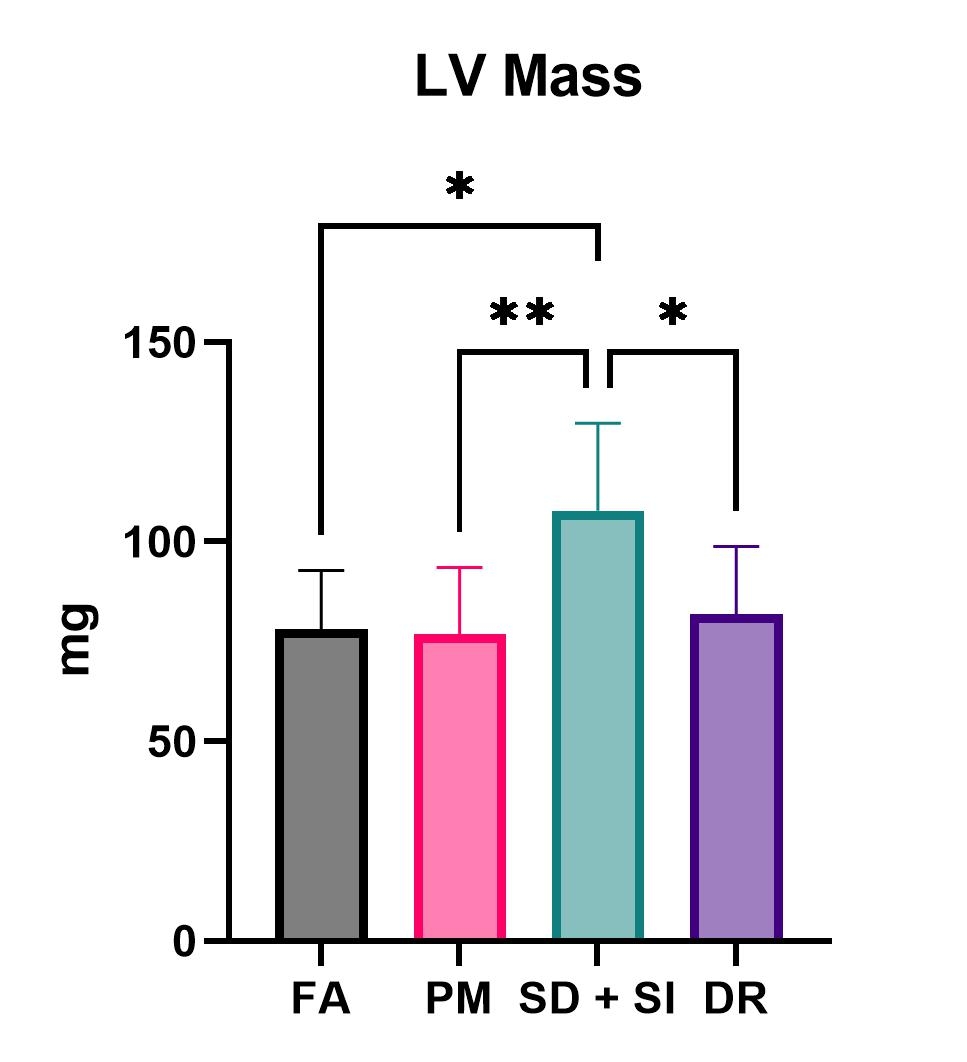
Abstract Body (Do not enter title and authors here): Background: Cardiovascular disease (CVD) remains the leading cause of death in the U.S., with major influence by environmental factors (Particulate Matter PM2.5 exposure), and psychosocial stress. These factors converge on shared biological pathways, including direct particle translocation, systemic inflammation, and oxidative stress, ultimately impacting cardiovascular and behavioral outcomes such as anxiety-like behavior and the hypothalamic-pituitary-adrenal (HPA) axis activation. Hypothesis: PM2.5 or psychosocial stress exposures can both have significant effects on the cardiovascular system. Methods: Male C57BL/6 mice were exposed to filtered air (FA) or PM ≤2.5 μm at concentrations of 34.85 μg/m3 for six hours/day, five days/week for three weeks. Mice underwent 10 minutes of physical interaction with a retired FVB breeder, followed by 18 hours of sensory (non-physical) contact (SDSI) for 10 days. For the Daily Restraint (DR) group, mice were placed in perforated conical tubes for 2 hours over 7 days. Data was analyzed using one-way ANOVA with significance set at p<0.05. Results: DR exposure significantly increased corticosterone levels (p<0.0001). Tail-cuff measurements exhibited a statistically significant reduction in both systolic and diastolic blood pressure for the DR group (p<0.05). Echocardiography revealed that left ventricular mass was significantly increased for the SDSI and DR groups. Ejection Fraction and Fractional Shortening were both significantly increased from the DR exposure (p<0.05). Pressure-volume (PV) loop analyses demonstrated that SDSI exposure caused an increase in the End-diastolic PV-relationship (p<0.05). Functional analyses of isolated cardiac myocytes revealed that PM2.5 and DR groups exhibited reduced contraction velocity under isoproterenol stimulation compared to FA (p<0.05). Additionally, these groups showed increased relaxation velocity under the same conditions (p<0.05). Conclusion: Chronic stress induced a compensatory cardiac response, marked by increased LV mass, elevated systolic function, and reduced blood pressure. Moreover, isolated cardiomyocytes showed impaired β-adrenergic contractility and relaxation. Elevated circulating corticosterone levels further indicate HPA axis activation; therefore, PM2.5 could also be considered a stressor. These findings suggest that early maladaptive remodeling occurs in the heart under chronic stress, highlighting its potential role in increasing long-term risk for CVD.
More abstracts on this topic:
A Machine Learning Approach to Simplify Risk Stratification of Patients with Atherosclerotic Cardiovascular Disease
Li Hsin Fang, Gluckman Ty, Nute Andrew, Weerasinghe Roshanthi, Wendt Staci, Wilson Eleni, Sidelnikov Eduard, Kathe Niranjan, Swihart Charissa, Jones Laney
A Potential Link Between Stress Kinase JNK2 and AKAP-1 in Catecholamine-Induced Acute Heart FailureKohli Aaryan, Yan Jiajie, Cao Yuanyuan, Bare Dan, Ai Xun