Final ID: MP1798
Navigating the Management of a Saphenous Vein Graft Aneurysm: A Case Report on Conservative Medical Management and Discussion of Treatment Options
Abstract Body (Do not enter title and authors here): Introduction
Saphenous vein graft (SVG) aneurysm is a rare but potentially serious late complication following coronary artery bypass grafting (CABG). The natural history is variable and the pathologic mechanism is poorly understood. It often is asymptomatic and incidentally found. Symptomatic patients can present with dyspnea, chest pain, or life-threatening rupture. Diagnosis is often made by CT and invasive coronary angiography. Management decisions for percutaneous or surgical interventions are guided by aneurysm size, risk of rupture and patient comorbidities.
Case Description
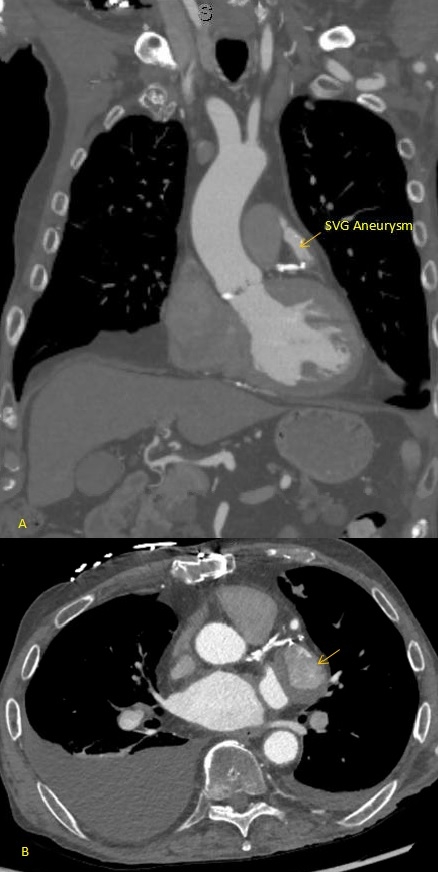
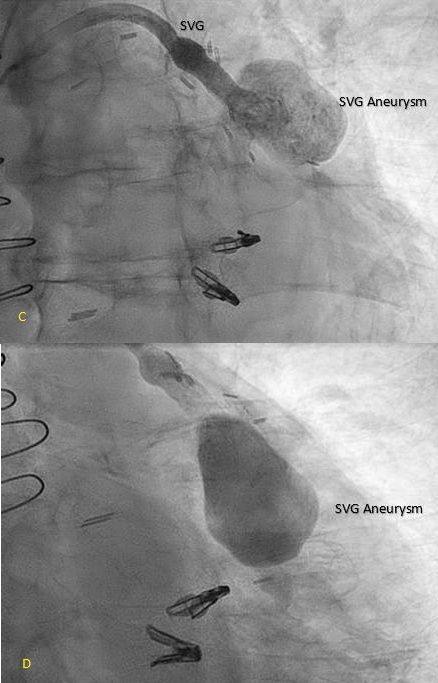
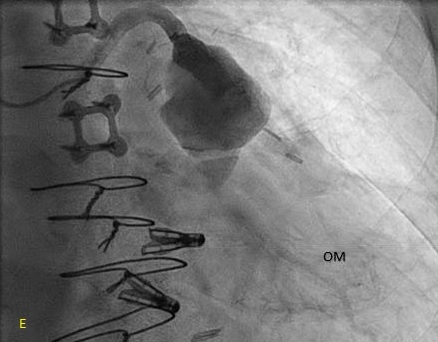
An 80-year-old patient with a history of coronary artery disease status post CABG in 2021, paroxysmal atrial fibrillation, heart failure with preserved ejection fraction, severe mitral regurgitation status post TEER-MitraClip, and moderate-to-severe aortic stenosis (aortic valve area 0.6 cm2, mean gradient 31 mmHg) presented with progressive exertional dyspnea, weakness, and lightheadedness. Transthoracic echocardiography confirmed moderate-to-severe aortic stenosis, and a cardiac CT was obtained for transcatheter aortic valve replacement (TAVR) evaluation. Imaging incidentally revealed a 3.1 cm SVG aneurysm with suspected intraluminal thrombus, prompting initiation of anticoagulation and left heart catheterization to further characterize the aneurysm.
Multidisciplinary Heart Team evaluation concluded that aortic stenosis was the primary contributor to symptoms. After a discussion of risks and benefits of SVG intervention options, the patient elected for conservative management with ongoing surveillance.
Discussion
SVG aneurysms are rare and pose a complex clinical challenge. A recent review offers proposed management strategies. Current management requires individualized treatment decisions based on patient risk, aneurysm type, size, presence of complications, whether symptomatic, and available expertise. The three current mainstays of treatment include observation and medical therapy, surgery and percutaneous intervention. Medical therapy and observation are preferred for patients that are high risk surgical candidates, or have multiple comorbidities. Percutaneous interventions are minimally invasive and include covered stents, coils, delivering endoluminal grafts and thrombin injections. Surgery is preferred for those that are hemodynamically unstable, and have acute significant complications. In our case, the patient met criteria and could be managed non-operatively.
Saphenous vein graft (SVG) aneurysm is a rare but potentially serious late complication following coronary artery bypass grafting (CABG). The natural history is variable and the pathologic mechanism is poorly understood. It often is asymptomatic and incidentally found. Symptomatic patients can present with dyspnea, chest pain, or life-threatening rupture. Diagnosis is often made by CT and invasive coronary angiography. Management decisions for percutaneous or surgical interventions are guided by aneurysm size, risk of rupture and patient comorbidities.
Case Description
An 80-year-old patient with a history of coronary artery disease status post CABG in 2021, paroxysmal atrial fibrillation, heart failure with preserved ejection fraction, severe mitral regurgitation status post TEER-MitraClip, and moderate-to-severe aortic stenosis (aortic valve area 0.6 cm2, mean gradient 31 mmHg) presented with progressive exertional dyspnea, weakness, and lightheadedness. Transthoracic echocardiography confirmed moderate-to-severe aortic stenosis, and a cardiac CT was obtained for transcatheter aortic valve replacement (TAVR) evaluation. Imaging incidentally revealed a 3.1 cm SVG aneurysm with suspected intraluminal thrombus, prompting initiation of anticoagulation and left heart catheterization to further characterize the aneurysm.
Multidisciplinary Heart Team evaluation concluded that aortic stenosis was the primary contributor to symptoms. After a discussion of risks and benefits of SVG intervention options, the patient elected for conservative management with ongoing surveillance.
Discussion
SVG aneurysms are rare and pose a complex clinical challenge. A recent review offers proposed management strategies. Current management requires individualized treatment decisions based on patient risk, aneurysm type, size, presence of complications, whether symptomatic, and available expertise. The three current mainstays of treatment include observation and medical therapy, surgery and percutaneous intervention. Medical therapy and observation are preferred for patients that are high risk surgical candidates, or have multiple comorbidities. Percutaneous interventions are minimally invasive and include covered stents, coils, delivering endoluminal grafts and thrombin injections. Surgery is preferred for those that are hemodynamically unstable, and have acute significant complications. In our case, the patient met criteria and could be managed non-operatively.
More abstracts on this topic:
Association of Pre-operative Neutrophil to Lymphocyte Ratio (NLR) and Post-operative AKI in Patients Undergoing CABG: A Meta-Analysis
Patel Bhavin, Lapsiwala Boney, Jariwala Prayag, Suresh Aditya, Vanani Samir, Patel Shaurya, Rajani Aayushi, Desai Rupak
A Novel Multivariate Scoring System for Diagnosing Post-Myocardial Infarction Pericarditis Following Percutaneous Coronary InterventionBolaji Olayiwola, Omoru Okiemute, Upreti Prakash, Echari Blanche, Shoar Saeed, Basit Jawad, Alraies M Chadi