Final ID: MP2117
Clot or Not? Witnessing the Power of Multimodality Imaging
Abstract Body (Do not enter title and authors here):
Background. Most left ventricular (LV) apical defects noted on transthoracic echocardiography (TTE) are presumed to be thrombi especially when an apical wall motion abnormality is concurrently present. This case report highlights the importance of multi-modality imaging in the work-up of an apical mass in the presence of wall motion abnormalities with an unexpected final diagnosis.
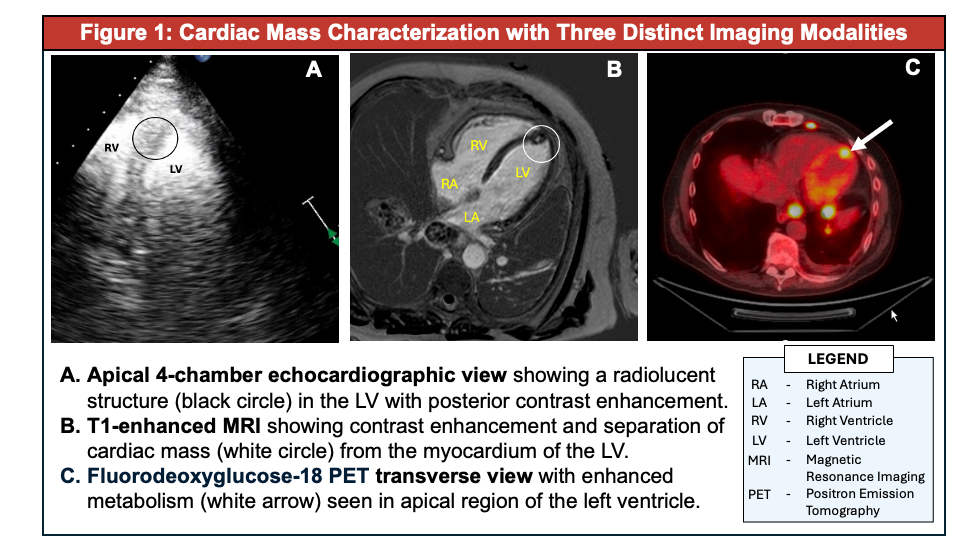
Case Presentation. A 67-year-old man with a past history of pleural mesothelioma complicated by pericardial effusions and atrial arrythmias now in partial remission, presented for a TTE pre-CAR-T Cell chemotherapy. The TTE was ordered for further evaluation of patient reported episodes of shortness of breath over the last 3 months despite active bevacizumab therapy. The TTE was notable for a normal LV ejection fraction (57%), anteroseptal and apical septal wall hypokinesis as well as a subtle density at the LV apex which appeared to take up microbubble contrast. (1A, circled). A restaging non-contrast computed tomography (CT) scan done 1 month prior demonstrated a pericardial nodule abutting the myocardium but did not show any intracardiac masses. To better characterize the mass, a cardiovascular magnetic resonance imaging study (CMR) was performed. On delayed enhancement the mass appeared heterogeneous with evidence of gadolinium contrast uptake. This ruled out the possibility of thrombus and suggested a vascular structure. (1B, circled). Subsequent cardiac positron emitted tomography (PET) scan with 11.6mCl F-18 fluorodeoxyglucose (F-FDG) demonstrated a hypermetabolic focus in the LV apex suspicious for metastatic deposit from known mesothelioma. Similar uptake was also noted in the lungs, pleura, and thoracoabdominal nodes. Suprarenal mass biopsy revealed malignant mesothelioma. (1C, arrow).
Discussion. Cardiac metastases of solid tumors are extremely rare. When they do occur, most are in the pericardium (~58%) followed by the myocardium (~19%), epicardium, and endocardium, respectively. In this patient, the TTE finding of microbubble contrast uptake in the LV apical mass was key to trigger further imaging with CMR and PET and ultimately diagnose metastases which would otherwise not have been discovered. Early discovery of recurrence and metastases improve chances for a better outcome. In patients with known history of malignancy, physicians should be vigilant in utilizing multi-modality imaging for intracardiac mass differentiation.
Background. Most left ventricular (LV) apical defects noted on transthoracic echocardiography (TTE) are presumed to be thrombi especially when an apical wall motion abnormality is concurrently present. This case report highlights the importance of multi-modality imaging in the work-up of an apical mass in the presence of wall motion abnormalities with an unexpected final diagnosis.
Case Presentation. A 67-year-old man with a past history of pleural mesothelioma complicated by pericardial effusions and atrial arrythmias now in partial remission, presented for a TTE pre-CAR-T Cell chemotherapy. The TTE was ordered for further evaluation of patient reported episodes of shortness of breath over the last 3 months despite active bevacizumab therapy. The TTE was notable for a normal LV ejection fraction (57%), anteroseptal and apical septal wall hypokinesis as well as a subtle density at the LV apex which appeared to take up microbubble contrast. (1A, circled). A restaging non-contrast computed tomography (CT) scan done 1 month prior demonstrated a pericardial nodule abutting the myocardium but did not show any intracardiac masses. To better characterize the mass, a cardiovascular magnetic resonance imaging study (CMR) was performed. On delayed enhancement the mass appeared heterogeneous with evidence of gadolinium contrast uptake. This ruled out the possibility of thrombus and suggested a vascular structure. (1B, circled). Subsequent cardiac positron emitted tomography (PET) scan with 11.6mCl F-18 fluorodeoxyglucose (F-FDG) demonstrated a hypermetabolic focus in the LV apex suspicious for metastatic deposit from known mesothelioma. Similar uptake was also noted in the lungs, pleura, and thoracoabdominal nodes. Suprarenal mass biopsy revealed malignant mesothelioma. (1C, arrow).
Discussion. Cardiac metastases of solid tumors are extremely rare. When they do occur, most are in the pericardium (~58%) followed by the myocardium (~19%), epicardium, and endocardium, respectively. In this patient, the TTE finding of microbubble contrast uptake in the LV apical mass was key to trigger further imaging with CMR and PET and ultimately diagnose metastases which would otherwise not have been discovered. Early discovery of recurrence and metastases improve chances for a better outcome. In patients with known history of malignancy, physicians should be vigilant in utilizing multi-modality imaging for intracardiac mass differentiation.
More abstracts on this topic:
A Diagnostic Pitfall: Subclavian Stenosis Mimicking Severe Aortic Stenosis on Echocardiography"
Ezaldin Shady, Abdelsalam Mahmoud, Elsayed Omar, Lee Marciano
A Novel Framework for End-Diastolic and End-Systolic Frame Localization in Contrast and Non-Contrast Echocardiography Without Manual AnnotationsPatel Sahaj, Arora Garima, Kummaragunta Neeraj, Yerabolu Krishin, Shahid Abdulla, Baria Priyank, Li Cynthia, Vekariya Nehal, Pampana Akhil, Arora Pankaj