Final ID: Su3111
Premature Discontinuation or Downtitration of Medical Therapy for Heart Failure After Changes in Kidney Function
Abstract Body (Do not enter title and authors here): Background: Despite the known benefits of guideline directed medical therapy (GDMT) for Heart Failure (HF), implementation of these therapies is often limited by concern for worsening kidney function. However, declines in estimated glomerular filtration rate (eGFR) are expected when initiating GDMT, and most declines in eGFR that are < 30% from baseline do not represent actual worsening kidney function. We aimed to determine the association between decline in eGFR and downtitration of GDMT among individuals with HF.
Methods: We conducted a retrospective analysis of adult patients with a diagnosis of HF and EF<=40% in a large, diverse health system with a new prescription for an angiotensin converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARB), angiotensin receptor neprilysin inhibitor (ARNI), mineralocorticoid receptor antagonist (MRA) or sodium glucose cotransporter 2 inhibitor (SGLT2i) between 4/1/2021-6/30/2024, and a baseline eGFR > 30 ml/min/1.73 m2 within 3 months prior. The primary exposure was change in eGFR measured between 1 week and 3 months following the GDMT prescription date, categorized as no change/improvement, 0-10%, 10-20%, 20-30% and >=30%. The primary outcome was discontinuation or down titration of GDMT. We performed a logistic regression analysis to calculate the odds ratio (95% confidence interval) of GDMT adjustment by eGFR change, adjusting for age, sex, and race/ethnicity, insurance type, nSES, other GDMT, and baseline eGFR.
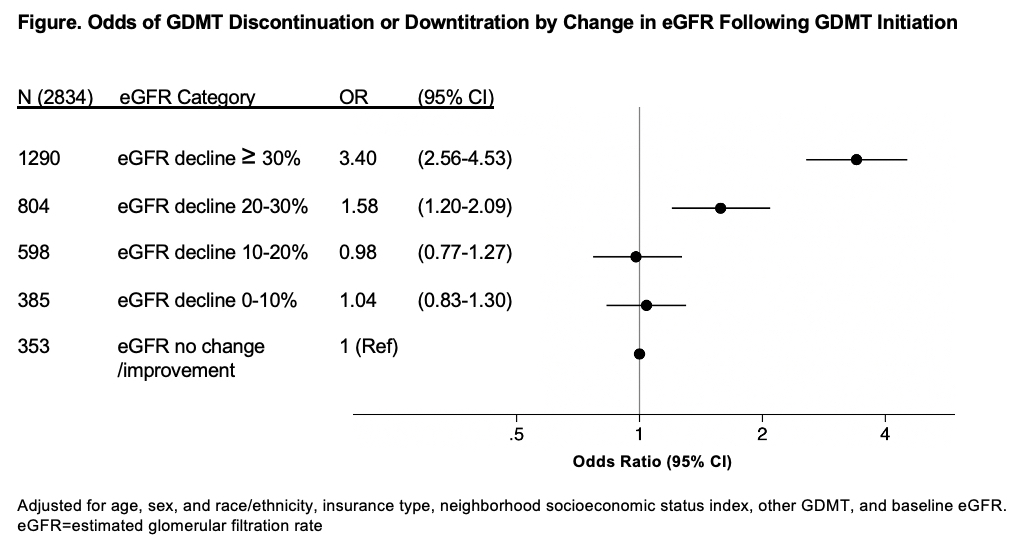
Results: A total of 2,834 individuals with HF (mean age 69.4 years, 32% female, 19% Black or African American) were started on a new GDMT and had subsequent eGFR monitoring. Compared to individuals with no change or improvement in eGFR there was no significant increase in the odds of GDMT discontinuation or down titration among those who experienced an eGFR decline of 0-10% or 10-20%. Individuals with an eGFR decline of 20-30% had 1.6 higher odds (95% CI 1.2-2.1) of GDMT downtitration and those with an eGFR decline of >=30% had a 3.4 higher odds (95% CI 2.6-4.5) compared to those with no eGFR change or improvement. (Figure)
Conclusions: We found that among individuals with HF, initiation of ACEi/ARB, ARNI, MRA or SGLT2i was associated with a higher odds of discontinuation or downtitration of the drug with an eGFR decline of 20-30%, which was likely not a clinically meaningful decline. Prescriber fear of kidney function decline may serve as a barrier to implementing GDMT among HF patients.
Methods: We conducted a retrospective analysis of adult patients with a diagnosis of HF and EF<=40% in a large, diverse health system with a new prescription for an angiotensin converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARB), angiotensin receptor neprilysin inhibitor (ARNI), mineralocorticoid receptor antagonist (MRA) or sodium glucose cotransporter 2 inhibitor (SGLT2i) between 4/1/2021-6/30/2024, and a baseline eGFR > 30 ml/min/1.73 m2 within 3 months prior. The primary exposure was change in eGFR measured between 1 week and 3 months following the GDMT prescription date, categorized as no change/improvement, 0-10%, 10-20%, 20-30% and >=30%. The primary outcome was discontinuation or down titration of GDMT. We performed a logistic regression analysis to calculate the odds ratio (95% confidence interval) of GDMT adjustment by eGFR change, adjusting for age, sex, and race/ethnicity, insurance type, nSES, other GDMT, and baseline eGFR.
Results: A total of 2,834 individuals with HF (mean age 69.4 years, 32% female, 19% Black or African American) were started on a new GDMT and had subsequent eGFR monitoring. Compared to individuals with no change or improvement in eGFR there was no significant increase in the odds of GDMT discontinuation or down titration among those who experienced an eGFR decline of 0-10% or 10-20%. Individuals with an eGFR decline of 20-30% had 1.6 higher odds (95% CI 1.2-2.1) of GDMT downtitration and those with an eGFR decline of >=30% had a 3.4 higher odds (95% CI 2.6-4.5) compared to those with no eGFR change or improvement. (Figure)
Conclusions: We found that among individuals with HF, initiation of ACEi/ARB, ARNI, MRA or SGLT2i was associated with a higher odds of discontinuation or downtitration of the drug with an eGFR decline of 20-30%, which was likely not a clinically meaningful decline. Prescriber fear of kidney function decline may serve as a barrier to implementing GDMT among HF patients.
More abstracts on this topic:
Effects of Sacubitril-Valsartan on Prevention of Cardiotoxicity in High-Risk Patients Undergoing Anthracycline Chemotherapy: A Double-Blind Randomized Placebo-Controlled Clinical Trial – The SARAH Trial
Bonatto Marcely, Zaninelli Maiolino Julyana, Mosko Larissa Arlete, Mialski Talita, Ota Tammy, Moura Lidia, Cauduro Sanderson, Bocchi Edimar, Ferreira Silvia, Avila Monica, Lechinewski Luka, Torres Rafael, Costa Amanda, Coiradas Andressa, Costa Nadya, Contin Lais
Effects of Empagliflozin on diuresis in heart failure: Results from the CINNAMON-study and in-vivo experimentsSinha Frederick, Klatt Susanne, Rietmann Alexander, Schoepperl Anna, Born Sebastian, Maier Lars, Schweda Frank, Wagner Stefan