Final ID: MP270
Mobilization in Patients with Cardiogenic Shock Requiring Temporary Mechanical Circulatory Support: Safety and Association with Functional Outcomes
Abstract Body (Do not enter title and authors here): Background: Early mobilization is recommended by guidelines for all patients with critical illness, yet its safety and efficacy in patients with cardiogenic shock (CS) requiring temporary mechanical circulatory support (tMCS) is not well-defined.
Methods: Secondary analysis of patients requiring prolonged (≥2 days) tMCS in a larger prospective observational study of CS survivors at 2 hospitals. CS severity was scored by Society of Cardiovascular Angiography and Interventions (SCAI) stages. Mobilization (i.e. physical therapy [PT] on tMCS) was classified as early (EM, initiated ≤2 days after tMCS placement), late (LM, >2 days after placement), or none. Mobility was rated by the Johns Hopkins Highest Level of Mobility (JH-HLM) scale, from 1 (lying in bed) to 8 (walking >250 ft) at initial and final ICU PT sessions. Disability was assessed by the modified Rankin scale (score ≥2 indicating disability) at discharge and 3-month follow-up. Adverse events (AEs) during mobilization on tMCS were assessed.
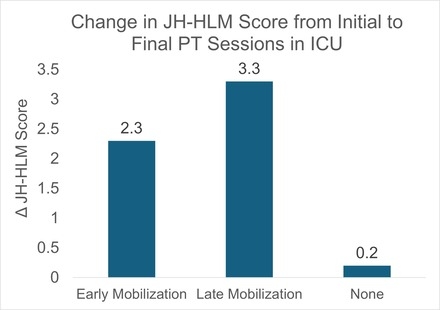
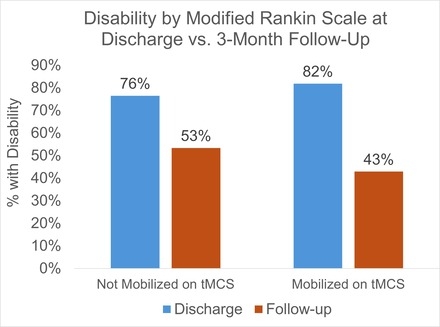
Results: Of 141 CS survivors, 39 required tMCS ≥2 days and were included in the analysis (average age 57 years, 5% women). Mobilization on tMCS was performed in 56% (26% EM, 31% LM). Among these patients, 59% had femoral device placement and 59% had axillary/central (18% switched configurations), while in those not mobilized on tMCS, 94% had femoral and 12% had axillary/central (6% switched). During the first PT session on tMCS, 95% of patients were in SCAI Stage D CS (vasoactive support and tMCS). Collectively, mobilized patients had 162 PT sessions on tMCS, with a median of 4.5 (Q1 2.3, Q3 8.8) sessions per patient, and one AE that required stopping PT (reduced cardiac output without increasing hemodynamic support). Mean (SD) change in JH-HLM score from initial to final PT assessment in the ICU was +2.3 (2.8) for EM, +3.3 (2.1) for LM, and +0.2 (1.3) for none (p<0.001) (Figure 1). Patients who were mobilized on tMCS had a greater reduction in disability from discharge to follow-up compared to those not mobilized on tMCS, though this was not statistically significant (Figure 2).
Conclusion: Mobilization in patients with tMCS was associated with a low rate of adverse events and significant improvements in ICU mobility. No vascular injury events were observed, though there is a low representation of women, who are at higher risk. Larger studies are needed to further examine the effect of ICU mobilization on post-ICU functional status in patients with CS requiring tMCS.
Methods: Secondary analysis of patients requiring prolonged (≥2 days) tMCS in a larger prospective observational study of CS survivors at 2 hospitals. CS severity was scored by Society of Cardiovascular Angiography and Interventions (SCAI) stages. Mobilization (i.e. physical therapy [PT] on tMCS) was classified as early (EM, initiated ≤2 days after tMCS placement), late (LM, >2 days after placement), or none. Mobility was rated by the Johns Hopkins Highest Level of Mobility (JH-HLM) scale, from 1 (lying in bed) to 8 (walking >250 ft) at initial and final ICU PT sessions. Disability was assessed by the modified Rankin scale (score ≥2 indicating disability) at discharge and 3-month follow-up. Adverse events (AEs) during mobilization on tMCS were assessed.
Results: Of 141 CS survivors, 39 required tMCS ≥2 days and were included in the analysis (average age 57 years, 5% women). Mobilization on tMCS was performed in 56% (26% EM, 31% LM). Among these patients, 59% had femoral device placement and 59% had axillary/central (18% switched configurations), while in those not mobilized on tMCS, 94% had femoral and 12% had axillary/central (6% switched). During the first PT session on tMCS, 95% of patients were in SCAI Stage D CS (vasoactive support and tMCS). Collectively, mobilized patients had 162 PT sessions on tMCS, with a median of 4.5 (Q1 2.3, Q3 8.8) sessions per patient, and one AE that required stopping PT (reduced cardiac output without increasing hemodynamic support). Mean (SD) change in JH-HLM score from initial to final PT assessment in the ICU was +2.3 (2.8) for EM, +3.3 (2.1) for LM, and +0.2 (1.3) for none (p<0.001) (Figure 1). Patients who were mobilized on tMCS had a greater reduction in disability from discharge to follow-up compared to those not mobilized on tMCS, though this was not statistically significant (Figure 2).
Conclusion: Mobilization in patients with tMCS was associated with a low rate of adverse events and significant improvements in ICU mobility. No vascular injury events were observed, though there is a low representation of women, who are at higher risk. Larger studies are needed to further examine the effect of ICU mobilization on post-ICU functional status in patients with CS requiring tMCS.
More abstracts on this topic:
An Unusual Presentation of Cerebellar Stroke Following the Removal of Microaxial Flow Pump
Liu Zi Qian, Alsheikh-kassim Mohammad, Karpenos Joseph, Frodey Kevin
Association between Pressure-Adjusted Heart Rate and Mortality in Cardiogenic ShockGinder Curtis, Jentzer Jacob, Guo Jianping, Van Diepen Sean, Katz Jason, Morrow David, Berg David