Final ID: Su2009
The importance of social and clinical variables as risk factors for 30-day readmissions following acute myocardial infarctions
Abstract Body (Do not enter title and authors here): Background: Hospital readmissions are costly, burdensome to patients, and are often preventable. Patients recovering from an acute myocardial infarction (AMI) face varying risks of readmission, which may be influenced by clinical, sociodemographic, and social determinants of health. There is a critical gap in evaluating social risk factors in modeling 30-day readmissions using electronic health record (EHR) data. A better understanding of these risk factors may help target specific interventions to mitigate disparate health outcomes.
Objective: The objective of this study was to examine the relationship between demographic, clinical, and social characteristics and the risk of 30-day hospital readmission following AMI.
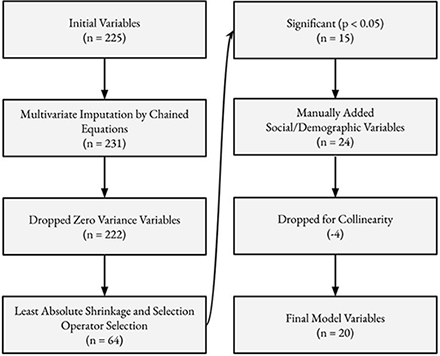
Methods: Patients admitted with an AMI to Vanderbilt University Medical Center between 2007 and 2016 were identified from a retrospective cohort of EHR data. Encounters were limited to index admissions among patients who were discharged alive. The outcome was 30-day hospital readmission. Variables included demographics (age, race, ethnicity), clinical characteristics (vitals, labs, comorbidities), and social risk factors (living alone, depression, dementia) and those with >70% missingness were excluded, and remaining missing values were imputed with multiple imputation. Variable selection for the final model is illustrated in Figure 1.
Results: A total of 6179 patients were included, and 646 experienced a 30-day readmission. The cohort included 4148 males, 1032 people of color, and the average age was 63.4 years. The top five statistically significant variables, based on magnitude of the odds ratio, included concurrent oncology care (OR: 4.92), medication non-compliance (OR: 4.67), sepsis in the 90 days before admission (OR: 4.46), length of stay of >= 5 days (OR: 3.169), and number of hospital admissions in the previous year (OR: 1.86). In addition, depression (OR: 1.32) or dementia (OR: 1.23) increased the risk for the outcome, while being Male (OR: 0.413) or non-Hispanic ethnicity (OR: 0.727) lowered the risk.
Conclusions: Using a longitudinal cohort of EHR data, clinical, demographic, and social variables were found to influence the risk of 30-day readmission following an AMI. Patient populations with clinical comorbidities, prior utilization of inpatient resources, and social risk factors, including medication non-compliance, or history of depression and dementia, may be essential groups to target for readmission reduction interventions.
Objective: The objective of this study was to examine the relationship between demographic, clinical, and social characteristics and the risk of 30-day hospital readmission following AMI.
Methods: Patients admitted with an AMI to Vanderbilt University Medical Center between 2007 and 2016 were identified from a retrospective cohort of EHR data. Encounters were limited to index admissions among patients who were discharged alive. The outcome was 30-day hospital readmission. Variables included demographics (age, race, ethnicity), clinical characteristics (vitals, labs, comorbidities), and social risk factors (living alone, depression, dementia) and those with >70% missingness were excluded, and remaining missing values were imputed with multiple imputation. Variable selection for the final model is illustrated in Figure 1.
Results: A total of 6179 patients were included, and 646 experienced a 30-day readmission. The cohort included 4148 males, 1032 people of color, and the average age was 63.4 years. The top five statistically significant variables, based on magnitude of the odds ratio, included concurrent oncology care (OR: 4.92), medication non-compliance (OR: 4.67), sepsis in the 90 days before admission (OR: 4.46), length of stay of >= 5 days (OR: 3.169), and number of hospital admissions in the previous year (OR: 1.86). In addition, depression (OR: 1.32) or dementia (OR: 1.23) increased the risk for the outcome, while being Male (OR: 0.413) or non-Hispanic ethnicity (OR: 0.727) lowered the risk.
Conclusions: Using a longitudinal cohort of EHR data, clinical, demographic, and social variables were found to influence the risk of 30-day readmission following an AMI. Patient populations with clinical comorbidities, prior utilization of inpatient resources, and social risk factors, including medication non-compliance, or history of depression and dementia, may be essential groups to target for readmission reduction interventions.
More abstracts on this topic:
An Evaluation of Stroke Literature Pamphlets For Stroke Patients
Degen Nathaniel, Sivakumar Milan, Varkey Thomas, Alexandrov Andrei, Singh Savdeep
Association between Polysocial Risk Score and Cardiovascular Health among Women of Reproductive Age in the American Heart Association’s Research Goes RedMetlock Faith, Kwapong Yaa, Vaidya Dhananjay, Evans Crystal, Ouyang Pamela, Commodore-mensah Yvonne, Sharma Garima