Final ID: MP352
Geospatial Mapping Reveals Racially Patterned Cardiometabolic Risk in Chicago Pharmacy Deserts
Abstract Body (Do not enter title and authors here):
Introduction:
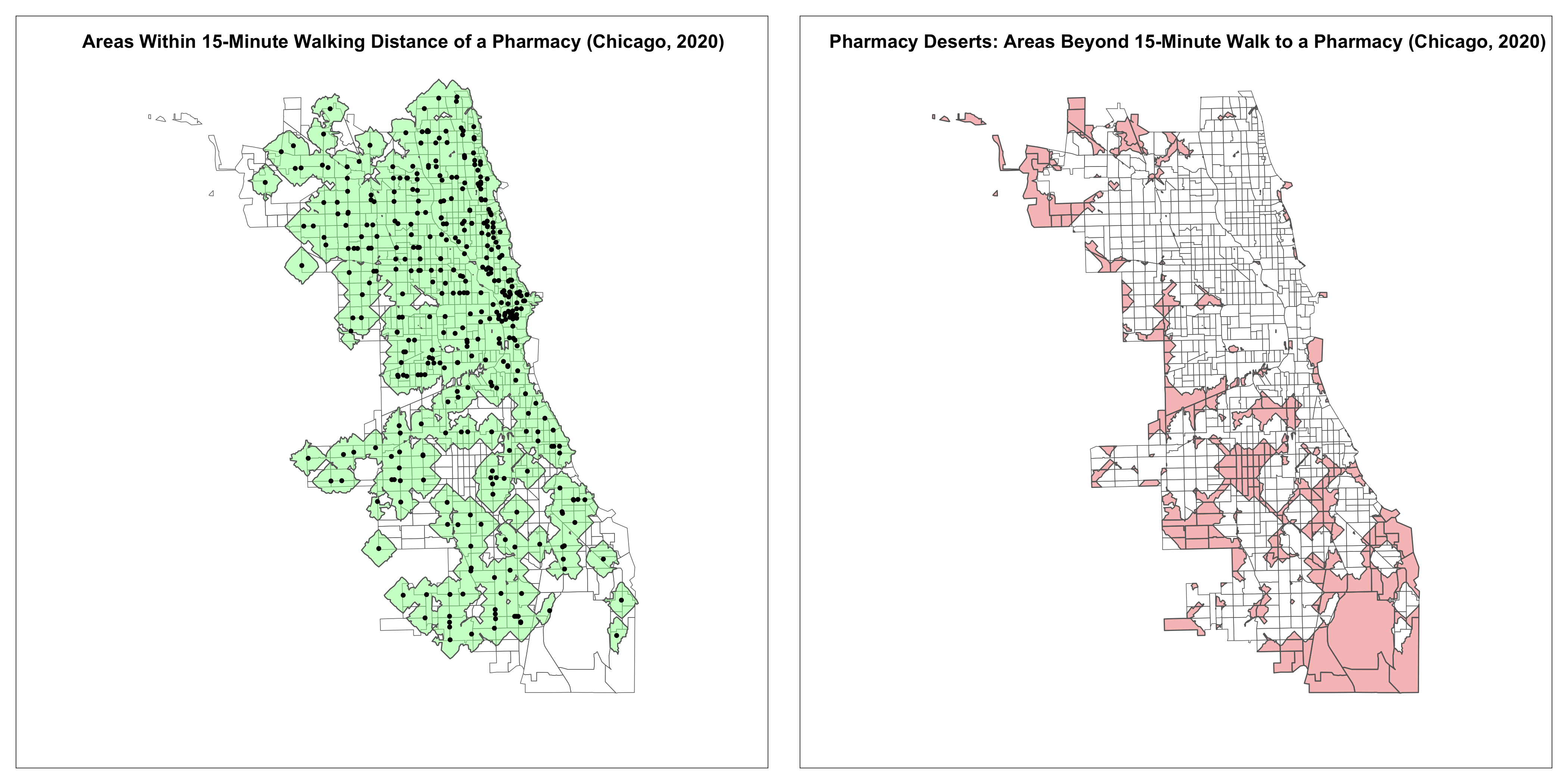
Pharmacy deserts, areas where residents lack nearby access to pharmacies, are a structural barrier to healthcare. Prior work has documented racial disparities in pharmacy access using census tracts, but such static measures do not capture accessibility metrics such as neighborhood walkability. Here, we introduce a novel geospatial method using 15-minute walking distances around active pharmacies to more precisely define pharmacy deserts (Figure 1). We then examine disparities in cardiometabolic control across racial groups in a large urban health system.
Hypothesis:
We hypothesized that living in a pharmacy desert is associated with worse cardiometabolic outcomes, and that this relationship varies by race.
Methods:
We conducted a cross-sectional analysis of Cardiology and Primary Care clinic patients at an urban tertiary care center between January 1, 2019, and December 31, 2023. We then modeled the odds of uncontrolled blood pressure (BP) and HbA1c by pharmacy desert residence in a case-control framework. Pharmacy data was obtained from the Chicago Data Portal and 15-minute walking distances were generated using Mapbox API. Patients living >15-minutes from a pharmacy were classified as living in a pharmacy desert. We used multivariable logistic regression to model uncontrolled BP (≥140/90 mmHg) and uncontrolled HbA1c (≥7.0%), adjusting for age, sex, and race, and testing for racial effect modification.
Results:
Among 20,504 patients with BP data, pharmacy desert residence was associated with higher odds of uncontrolled BP (OR = 1.11, p = 0.006). This association was significant among White patients (OR = 1.44, p = 0.001) but not Black patients (OR = 1.07, p = 0.13). A similar pattern was seen for HbA1c (N = 1,346): White patients had significantly higher odds of uncontrolled HbA1c in pharmacy deserts (OR = 2.93, p = 0.03), but Black patients did not (OR = 1.04, p = 0.79). Notably, Black patients had markedly worse control overall compared to white patients (BP OR = 2.11, p < 0.001; HbA1c OR = 1.60, p = 0.03), regardless of pharmacy access.
Conclusion:
Pharmacy deserts are linked to worse cardiometabolic outcomes for White patients, but this association is absent among Black patients, who consistently show poorer outcomes regardless of proximity to a pharmacy. These results suggest other factors may blunt the benefits of geographic proximity to a pharmacy among some racial groups.
Introduction:
Pharmacy deserts, areas where residents lack nearby access to pharmacies, are a structural barrier to healthcare. Prior work has documented racial disparities in pharmacy access using census tracts, but such static measures do not capture accessibility metrics such as neighborhood walkability. Here, we introduce a novel geospatial method using 15-minute walking distances around active pharmacies to more precisely define pharmacy deserts (Figure 1). We then examine disparities in cardiometabolic control across racial groups in a large urban health system.
Hypothesis:
We hypothesized that living in a pharmacy desert is associated with worse cardiometabolic outcomes, and that this relationship varies by race.
Methods:
We conducted a cross-sectional analysis of Cardiology and Primary Care clinic patients at an urban tertiary care center between January 1, 2019, and December 31, 2023. We then modeled the odds of uncontrolled blood pressure (BP) and HbA1c by pharmacy desert residence in a case-control framework. Pharmacy data was obtained from the Chicago Data Portal and 15-minute walking distances were generated using Mapbox API. Patients living >15-minutes from a pharmacy were classified as living in a pharmacy desert. We used multivariable logistic regression to model uncontrolled BP (≥140/90 mmHg) and uncontrolled HbA1c (≥7.0%), adjusting for age, sex, and race, and testing for racial effect modification.
Results:
Among 20,504 patients with BP data, pharmacy desert residence was associated with higher odds of uncontrolled BP (OR = 1.11, p = 0.006). This association was significant among White patients (OR = 1.44, p = 0.001) but not Black patients (OR = 1.07, p = 0.13). A similar pattern was seen for HbA1c (N = 1,346): White patients had significantly higher odds of uncontrolled HbA1c in pharmacy deserts (OR = 2.93, p = 0.03), but Black patients did not (OR = 1.04, p = 0.79). Notably, Black patients had markedly worse control overall compared to white patients (BP OR = 2.11, p < 0.001; HbA1c OR = 1.60, p = 0.03), regardless of pharmacy access.
Conclusion:
Pharmacy deserts are linked to worse cardiometabolic outcomes for White patients, but this association is absent among Black patients, who consistently show poorer outcomes regardless of proximity to a pharmacy. These results suggest other factors may blunt the benefits of geographic proximity to a pharmacy among some racial groups.
More abstracts on this topic:
Assessing Health Literacy and the Role of Race and Social Determinants in Cardiac Patients.
Odigwe Celestine, Lakkis Nasser, Mayfield Hanna, Mulyala Rajasekhar, Riad Mariam, Malik Hajira, Ruiz Brent, Mulekar Madhuri, Malozzi Christopher, Omar Bassam
A Retrospective Analysis of Chronic Kidney Disease and Arrhythmias-Related Mortality Among Adults in the United States (1999-2020): Insights into Disparities by Gender, Race/Ethnicity, and GeographyWaseem Neha, Nouman Zainab, Chaudhry Sohaib Aftab Ahmad, Tariq Waleed, Khan Iftikhar, Shah Mazhar, Farooqi Hanzala Ahmed, Faiz Muneeb