Final ID: MP1946
Left Pulmonary vein thrombosis following Lobectomy in a patient with Atrial fibrillation: a unique contraindication to cardioversion
Abstract Body (Do not enter title and authors here): Case presentation:
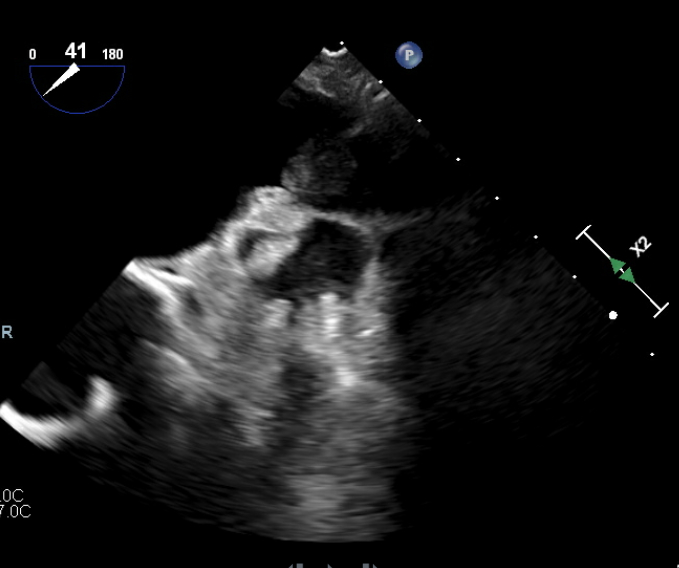
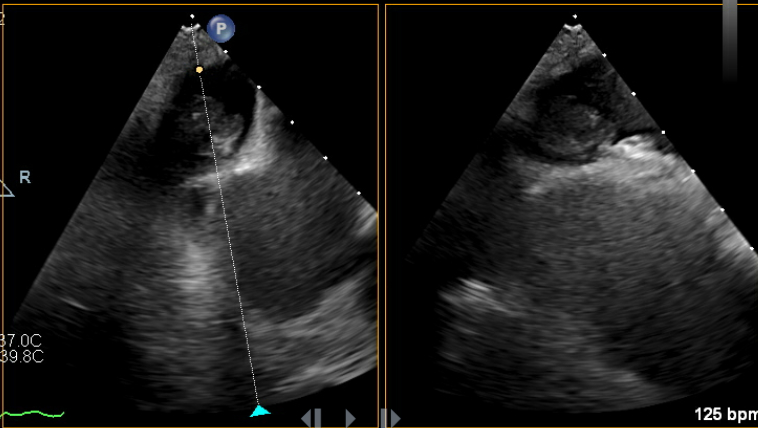
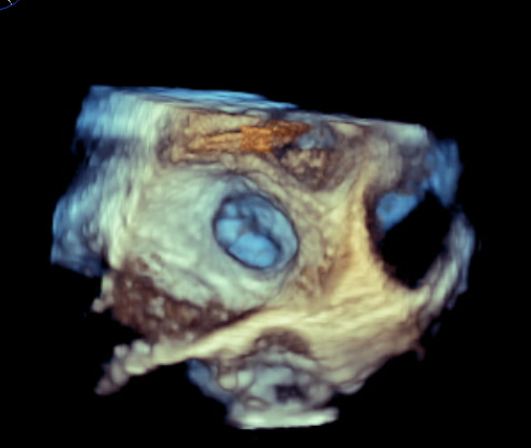
82-year-old male who presented with symptoms of progressively worsening shortness of breath and palpitations for 4 days. He was recently diagnosed with non-small cell carcinoma and underwent a left upper lobectomy a few months prior. Upon arrival, patient was tachycardic, with a heart rate in the 140s, requiring 5-6 L nasal cannula to maintain oxygen saturation above 92%. EKG revealed new onset atrial fibrillation with rapid ventricular response. Laboratory testing was remarkable for elevated NT-pro BNP to 4,000. CXR revealed bilateral pulmonary congestion consistent with pulmonary edema. Transthoracic echocardiogram was significant for severely reduced EF to 15-20%, previously normal. The patient was admitted for management of new onset-atrial fibrillation & HFrEF likely due to tachycardia-mediated cardiomyopathy. Cardioversion was initially planned; however transesophageal echocardiogram revealed an unexpected thrombus at the os of the left superior pulmonary vein. No thrombus was seen in the left atrial appendage. The patient was started on IV digoxin and low-dose esmolol drip for rate control along with a heparin drip for anticoagulation. However, the patient had sinus pauses for up to 5 seconds on esmolol drip. Given the limitation to control the heart rate, the patient underwent placement of CRT-P device. He was medically optimized and discharged with plan for outpatient cardioversion vs Atrial fibrillation ablation.
Discussion:
Atrial fibrillation with rapid ventricular response is a common precipitant of heart failure, often requiring rhythm control. The presence of intracardiac thrombus is a well-established contraindication due to the risk of systemic embolization. While most thrombi form in the left atrial appendage, our patient was found to have a thrombus in the left superior pulmonary vein, a unique and exceedingly rare finding. Most cases of pulmonary vein thrombosis are seen after catheter ablation, lobectomy, Lung transplantation, etc. Our case presented a unique dilemma due to the lack of guidelines addressing thromboembolic risk and cardioversion in this context. Therefore, a conservative approach was chosen with rate control and systemic anticoagulation. This case also highlights the value of comprehensive imaging like transesophageal echocardiography for through evaluation of pulmonary vein ostia in addition to left atrial appendage thrombus, especially in the context of recent thoracic surgery.
82-year-old male who presented with symptoms of progressively worsening shortness of breath and palpitations for 4 days. He was recently diagnosed with non-small cell carcinoma and underwent a left upper lobectomy a few months prior. Upon arrival, patient was tachycardic, with a heart rate in the 140s, requiring 5-6 L nasal cannula to maintain oxygen saturation above 92%. EKG revealed new onset atrial fibrillation with rapid ventricular response. Laboratory testing was remarkable for elevated NT-pro BNP to 4,000. CXR revealed bilateral pulmonary congestion consistent with pulmonary edema. Transthoracic echocardiogram was significant for severely reduced EF to 15-20%, previously normal. The patient was admitted for management of new onset-atrial fibrillation & HFrEF likely due to tachycardia-mediated cardiomyopathy. Cardioversion was initially planned; however transesophageal echocardiogram revealed an unexpected thrombus at the os of the left superior pulmonary vein. No thrombus was seen in the left atrial appendage. The patient was started on IV digoxin and low-dose esmolol drip for rate control along with a heparin drip for anticoagulation. However, the patient had sinus pauses for up to 5 seconds on esmolol drip. Given the limitation to control the heart rate, the patient underwent placement of CRT-P device. He was medically optimized and discharged with plan for outpatient cardioversion vs Atrial fibrillation ablation.
Discussion:
Atrial fibrillation with rapid ventricular response is a common precipitant of heart failure, often requiring rhythm control. The presence of intracardiac thrombus is a well-established contraindication due to the risk of systemic embolization. While most thrombi form in the left atrial appendage, our patient was found to have a thrombus in the left superior pulmonary vein, a unique and exceedingly rare finding. Most cases of pulmonary vein thrombosis are seen after catheter ablation, lobectomy, Lung transplantation, etc. Our case presented a unique dilemma due to the lack of guidelines addressing thromboembolic risk and cardioversion in this context. Therefore, a conservative approach was chosen with rate control and systemic anticoagulation. This case also highlights the value of comprehensive imaging like transesophageal echocardiography for through evaluation of pulmonary vein ostia in addition to left atrial appendage thrombus, especially in the context of recent thoracic surgery.
More abstracts on this topic:
A Case of Spike-on-T Phenomenon and Polymorphic Ventricular Tachycardia
Tran Brittany, Thimmiah Harun, Rosenthal Lawrence
A Growing Burden of Electronic Medical Record Messages in ACHD CareDailey Schwartz Andrew, Alegria Jorge