Final ID: Sa2067
Healthcare resource use (HCRU) and costs differ between those with and without follow-up LDL-C monitoring after newly initiating lipid lowering therapy (LLT)
Abstract Body (Do not enter title and authors here): Introduction/Background:
Despite wide availability of safe and effective LLT to reduce LDL-C and prevent ASCVD events, LLT is underused. There is evidence that LDL-C monitoring remains suboptimal in practice, but the association between lipid monitoring and HCRU is less clear.
Research Questions/Hypothesis:
In patients newly starting LLT, what is the association between LDL-C monitoring and clinical events and HCRU?
Methods/Approach:
Using TriNetX EMR data linked to PurpleLab claims from 2016 to 2023, we assessed a sample of insured US adults who newly initiated LLT. Index was defined as LLT initiation following a ≥6mo active baseline period with no prior LLT use. Patient characteristics were summarized, and standardized HCRU and healthcare charges were reported. Generalized linear models (GLM) estimated the independent association between LDL-C monitoring and HCRU (negative binomial regression) and total healthcare costs (Gamma regression) adjusting for key patient characteristics.
Results/Data:
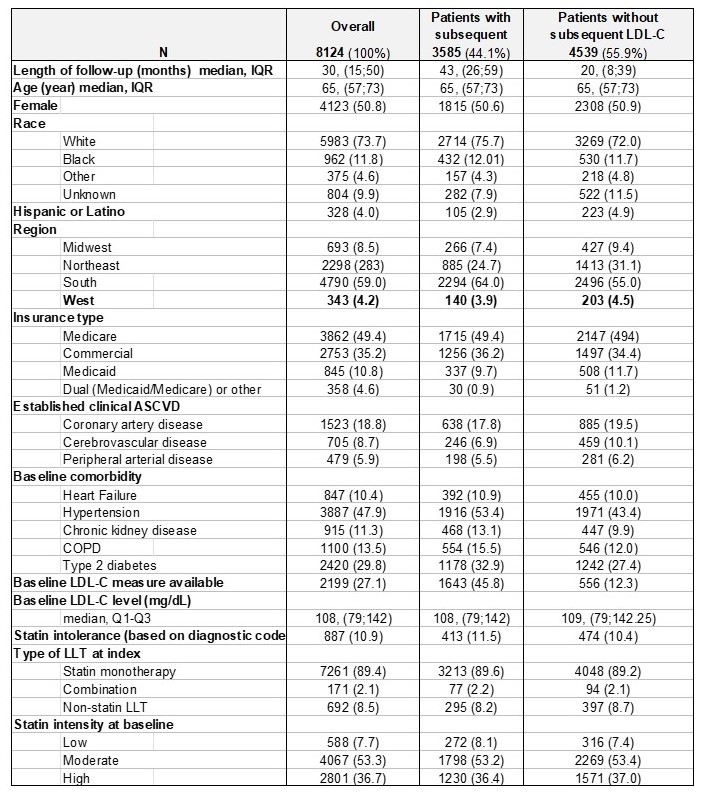
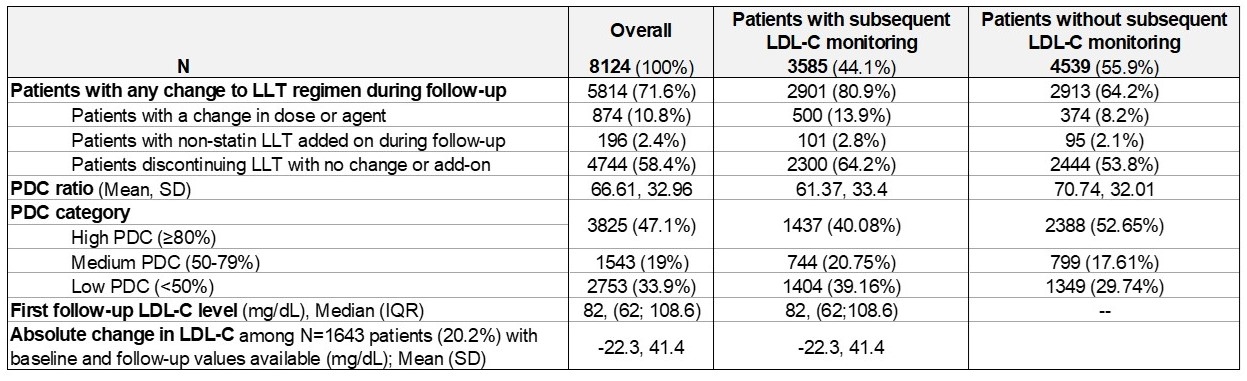
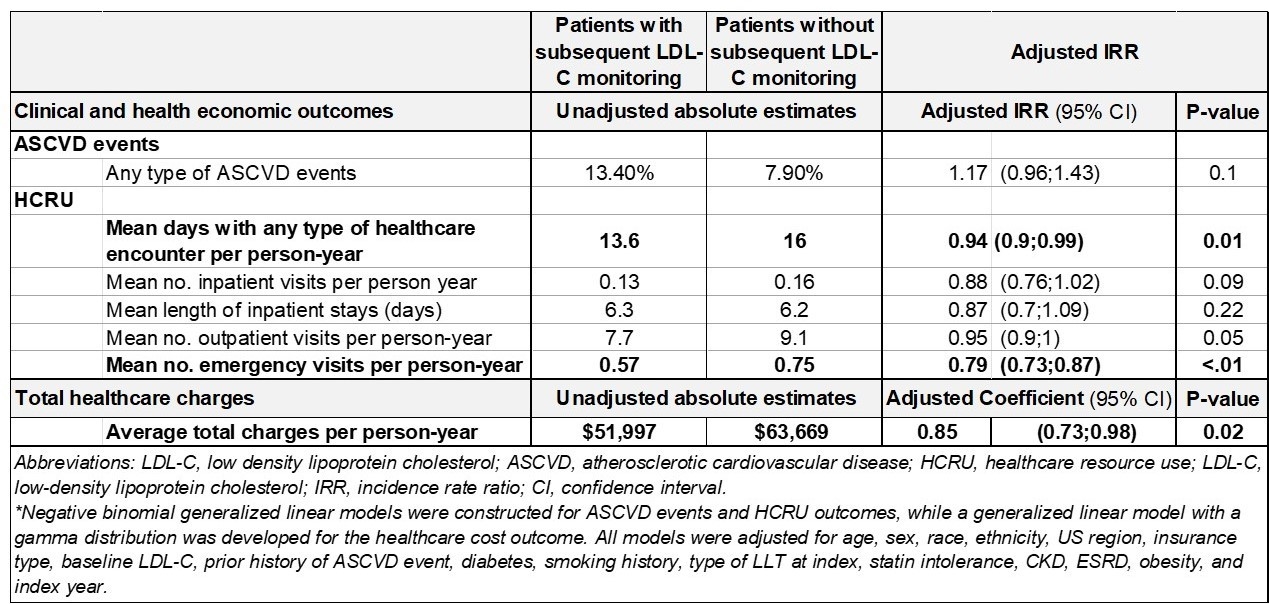
Among 8,124 adults starting LLT, the median (IQR) age was 65 (57,73), with 51% women. Adults undergoing LDL-C monitoring were more likely to have common comorbidities including hypertension, diabetes, COPD, and CKD (Table 1). Median baseline LDL-C was 108 mg/dL among those with values available. Overall, 56% of patients had no record of LDL-C testing after starting LLT over a 2.5-year median follow-up. Patients with monitoring during follow-up had nearly double the crude rate of ASCVD events (13.4% vs. 7.9%), but had fewer inpatient, outpatient, and emergency visits, and had lower total healthcare charges per person-year ($51,997 vs. $63,669) compared to those without (Table 2). After adjustment, there was no significant association between LDL-C monitoring and incident ASCVD events or inpatient visits, or HCRU overall. However, those without any LDL-C monitoring after starting LLT had 21% more emergency visits and 15% higher total healthcare costs even after adjusting for key characteristics (Table 2).
Conclusion(s):
LDL-C monitoring is suboptimal and those with follow-up testing often have other CV risk enhancers and comorbidities. Despite higher crude and similar adjusted ASCVD event rates, those with monitoring had fewer emergency visits and lower healthcare costs even after adjustment. LDL-C monitoring may be a proxy for engagement with preventive healthcare. Improving LDL-C monitoring may close gaps in preventable HCRU, with potential savings to health systems.
Despite wide availability of safe and effective LLT to reduce LDL-C and prevent ASCVD events, LLT is underused. There is evidence that LDL-C monitoring remains suboptimal in practice, but the association between lipid monitoring and HCRU is less clear.
Research Questions/Hypothesis:
In patients newly starting LLT, what is the association between LDL-C monitoring and clinical events and HCRU?
Methods/Approach:
Using TriNetX EMR data linked to PurpleLab claims from 2016 to 2023, we assessed a sample of insured US adults who newly initiated LLT. Index was defined as LLT initiation following a ≥6mo active baseline period with no prior LLT use. Patient characteristics were summarized, and standardized HCRU and healthcare charges were reported. Generalized linear models (GLM) estimated the independent association between LDL-C monitoring and HCRU (negative binomial regression) and total healthcare costs (Gamma regression) adjusting for key patient characteristics.
Results/Data:
Among 8,124 adults starting LLT, the median (IQR) age was 65 (57,73), with 51% women. Adults undergoing LDL-C monitoring were more likely to have common comorbidities including hypertension, diabetes, COPD, and CKD (Table 1). Median baseline LDL-C was 108 mg/dL among those with values available. Overall, 56% of patients had no record of LDL-C testing after starting LLT over a 2.5-year median follow-up. Patients with monitoring during follow-up had nearly double the crude rate of ASCVD events (13.4% vs. 7.9%), but had fewer inpatient, outpatient, and emergency visits, and had lower total healthcare charges per person-year ($51,997 vs. $63,669) compared to those without (Table 2). After adjustment, there was no significant association between LDL-C monitoring and incident ASCVD events or inpatient visits, or HCRU overall. However, those without any LDL-C monitoring after starting LLT had 21% more emergency visits and 15% higher total healthcare costs even after adjusting for key characteristics (Table 2).
Conclusion(s):
LDL-C monitoring is suboptimal and those with follow-up testing often have other CV risk enhancers and comorbidities. Despite higher crude and similar adjusted ASCVD event rates, those with monitoring had fewer emergency visits and lower healthcare costs even after adjustment. LDL-C monitoring may be a proxy for engagement with preventive healthcare. Improving LDL-C monitoring may close gaps in preventable HCRU, with potential savings to health systems.
More abstracts on this topic:
A Novel Machine Learning Strategy to Integrate Multi-Omics Data and Detect Genomic Loci and Gene-Environment Interactions for LDL Cholesterol
Li Changwei, Zhang Ruiyuan, Sun Yixi, Chen Jing, Wang Tao, Bazzano Lydia, Kelly Tanika, He Jiang
Assessing the Efficacy and Safety of Olezarsen in Lowering Triglyceride Levels: A Systematic Review and Meta-AnalysisShahzad Zoha, Batool Asma, Ijaz Osama, Rao Asad Gul, Rasool Warda, Wani Shariq Ahmad, Rauf Faateh, Ilmaguook Badr, Khan Arslan Ahmed, Bhatti Ali Hanif