Final ID: Mo3130
Outcomes of Supraclavicular Access in Temporary Pacemaker Implantation
Abstract Body (Do not enter title and authors here): Background: Temporary pacemakers (TPM) are often placed using femoral, jugular, or subclavian veins, but these approaches have risks like pneumothorax or lead dislodgement. The supraclavicular route may offer a safer alternative, but data is limited.
Methods: In this retrospective observational study, we assessed 3,569 patients who got a TPM at a tertiary hospital (2020–2024). Of these, 1,644 had supraclavicular access, and 1,925 had infraclavicular access. We compared success rates, complications, and procedure times. Data came from medical records, and all analyses were performed using SPSS v26.
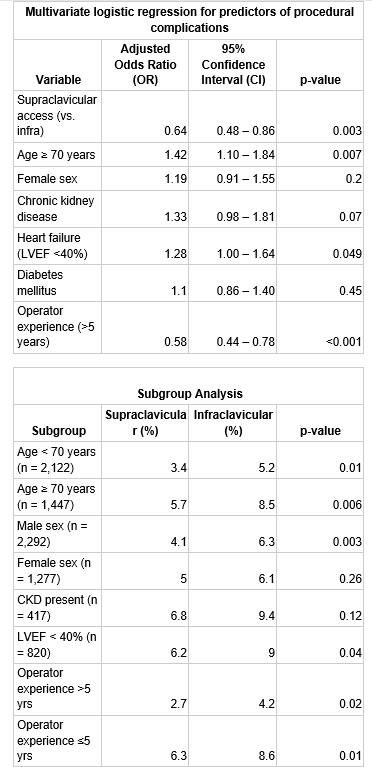
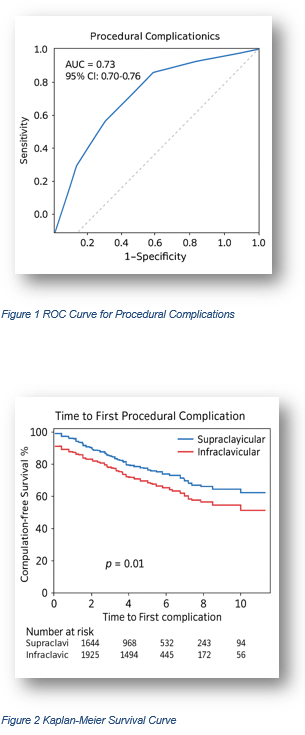
Results: The study compared outcomes between supraclavicular (n=1,644) and infraclavicular (n=1,925) approaches for temporary pacemaker implantation in 3,569 patients. Baseline characteristics were well-matched between groups, with similar age (63.7 vs 64.1 years), sex distribution (56.3% vs 55.7% male), and comorbidity profiles (all p>0.05). The supraclavicular approach demonstrated superior safety outcomes, with significantly lower overall complication rates (9.3% vs 14.8%, p<0.001), including reduced arterial puncture (2.0% vs 4.2%), pneumothorax (0.3% vs 1.1%), lead dislodgement (4.5% vs 6.8%), and hematoma formation (1.5% vs 2.7%). Multivariate analysis identified supraclavicular access as independently protective against complications (OR 0.59, 95% CI 0.48-0.73), along with younger age and normal renal function. Procedural efficiency favored the supraclavicular approach, with shorter mean procedure times (24.6 vs 29.1 minutes, p<0.001) and higher first-attempt success rates (89.4% vs 83.2%, p<0.001). Predictive modeling showed excellent discrimination for complications (AUC 0.73), while survival analysis confirmed prolonged complication-free intervals with supraclavicular access (log-rank p=0.01).
Conclusion: Supraclavicular access for TPM is safer, faster, and more successful than the traditional infraclavicular approach. It should be considered as a first-choice method, especially in emergencies.
Methods: In this retrospective observational study, we assessed 3,569 patients who got a TPM at a tertiary hospital (2020–2024). Of these, 1,644 had supraclavicular access, and 1,925 had infraclavicular access. We compared success rates, complications, and procedure times. Data came from medical records, and all analyses were performed using SPSS v26.
Results: The study compared outcomes between supraclavicular (n=1,644) and infraclavicular (n=1,925) approaches for temporary pacemaker implantation in 3,569 patients. Baseline characteristics were well-matched between groups, with similar age (63.7 vs 64.1 years), sex distribution (56.3% vs 55.7% male), and comorbidity profiles (all p>0.05). The supraclavicular approach demonstrated superior safety outcomes, with significantly lower overall complication rates (9.3% vs 14.8%, p<0.001), including reduced arterial puncture (2.0% vs 4.2%), pneumothorax (0.3% vs 1.1%), lead dislodgement (4.5% vs 6.8%), and hematoma formation (1.5% vs 2.7%). Multivariate analysis identified supraclavicular access as independently protective against complications (OR 0.59, 95% CI 0.48-0.73), along with younger age and normal renal function. Procedural efficiency favored the supraclavicular approach, with shorter mean procedure times (24.6 vs 29.1 minutes, p<0.001) and higher first-attempt success rates (89.4% vs 83.2%, p<0.001). Predictive modeling showed excellent discrimination for complications (AUC 0.73), while survival analysis confirmed prolonged complication-free intervals with supraclavicular access (log-rank p=0.01).
Conclusion: Supraclavicular access for TPM is safer, faster, and more successful than the traditional infraclavicular approach. It should be considered as a first-choice method, especially in emergencies.
More abstracts on this topic:
A Genome-wide CRISPRi Screen Implicates Coronary Artery Disease GWAS Genes as Key Regulators of Adventitial Fibroblast Proliferation
Jackson William, Zhu Ashley, Gu Wenduo, Berezowitz Alexa, Iyer Meghana, Cheng Paul
Clonal Fate Mapping of Sinoatrial Node ProgenitorsKethana Khushi, Black Brian, Galang Giselle, Chouhan Gagandeep, Mandla Ravi, Sinha Tanvi, Devine Walter, Mohan Rajiv, Soe Amanda, Vedantham Vasanth