Final ID: Sa2020
Evolving Disparities in Cardiomyopathy and Liver Disease Mortality Over Two Decades: A National Analysis by Race and Gender
Abstract Body (Do not enter title and authors here): Background
Cardiomyopathy and liver diseases are recognized as interrelated conditions due to their shared mechanisms, including systemic inflammation, neurohormonal dysregulation, and metabolic disturbances. While their mortality trends have been studied, there is a lack of national-level data on the intersection of these two conditions. Understanding the evolution of mortality patterns when both conditions coexist is crucial for identifying high-risk populations.
Research Question
We aimed to investigate national mortality trends and demographic disparities among U.S. adults with both cardiomyopathy and liver disease listed on their death certificates from 1999 to 2020.
Methods
We queried the CDC WONDER multiple cause-of-death database (1999–2020) for adults aged ≥25 years with ICD-10 codes for Cardiomyopathy (I42.x) and Liver Diseases (K70–K76). Age-adjusted mortality rates (AAMRs) were calculated using the 2000 U.S. standard population. Joinpoint regression identified inflection years and annual percent changes (APCs). Negative binomial regression estimated incidence rate ratios (IRRs), adjusting for age, sex, and race.
Results
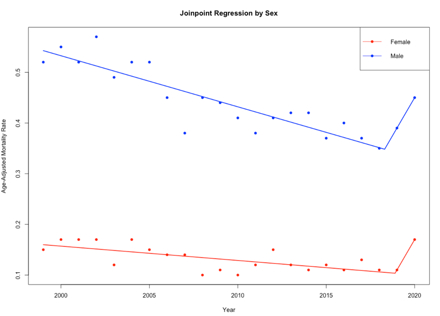
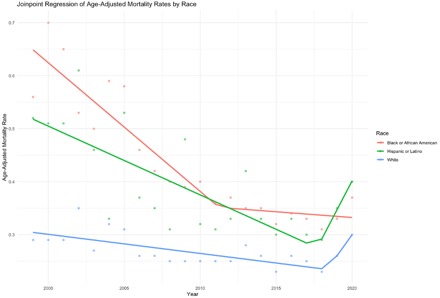
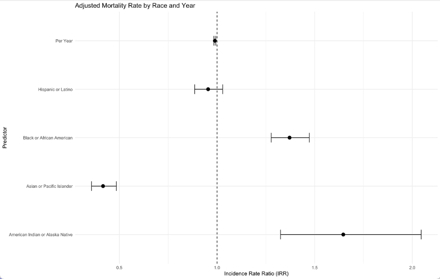
A total of 104,684 deaths involved both conditions. AAMRs declined from 2.39 in 1999 to 1.64 in 2018 (APC −1.9%, p<0.05), then rose to 2.31 in 2020 (APC +19.5%, p<0.01). Males had higher AAMRs than females, but the mortality trend reversed for both males (−1.01%/y to +6.00%/y) and females (−0.82% to +2.06%) in 2018. By race, Native Americans had the highest AAMR in 2020 (4.84), followed by Black (2.65), White (2.12), and Asian/Pacific Islander (0.93) groups. Disparities widened after 2018. Adjusted IRRs confirmed an elevated risk among American Indian/Alaska Native (1.65, 95% CI: 1.52–1.79) and Black individuals (1.37, 95% CI: 1.30–1.44), with a lower risk in Asian/Pacific Islanders (0.42, 95% CI: 0.38–0.46). Each year showed a 1.1% decline in risk (IRR 0.989, p < 0.001) before the reversal.
Conclusion
After two decades of decline, mortality involving both cardiomyopathy and liver disease rose sharply after 2018, especially among males and Native American and Black populations. This concerning trend may reflect increases in alcohol-related and metabolic liver disease, widening disparities in care, and pandemic-related disruptions. Targeted public health efforts are needed to address this dual burden and mitigate emerging cardiometabolic disparities.
Cardiomyopathy and liver diseases are recognized as interrelated conditions due to their shared mechanisms, including systemic inflammation, neurohormonal dysregulation, and metabolic disturbances. While their mortality trends have been studied, there is a lack of national-level data on the intersection of these two conditions. Understanding the evolution of mortality patterns when both conditions coexist is crucial for identifying high-risk populations.
Research Question
We aimed to investigate national mortality trends and demographic disparities among U.S. adults with both cardiomyopathy and liver disease listed on their death certificates from 1999 to 2020.
Methods
We queried the CDC WONDER multiple cause-of-death database (1999–2020) for adults aged ≥25 years with ICD-10 codes for Cardiomyopathy (I42.x) and Liver Diseases (K70–K76). Age-adjusted mortality rates (AAMRs) were calculated using the 2000 U.S. standard population. Joinpoint regression identified inflection years and annual percent changes (APCs). Negative binomial regression estimated incidence rate ratios (IRRs), adjusting for age, sex, and race.
Results
A total of 104,684 deaths involved both conditions. AAMRs declined from 2.39 in 1999 to 1.64 in 2018 (APC −1.9%, p<0.05), then rose to 2.31 in 2020 (APC +19.5%, p<0.01). Males had higher AAMRs than females, but the mortality trend reversed for both males (−1.01%/y to +6.00%/y) and females (−0.82% to +2.06%) in 2018. By race, Native Americans had the highest AAMR in 2020 (4.84), followed by Black (2.65), White (2.12), and Asian/Pacific Islander (0.93) groups. Disparities widened after 2018. Adjusted IRRs confirmed an elevated risk among American Indian/Alaska Native (1.65, 95% CI: 1.52–1.79) and Black individuals (1.37, 95% CI: 1.30–1.44), with a lower risk in Asian/Pacific Islanders (0.42, 95% CI: 0.38–0.46). Each year showed a 1.1% decline in risk (IRR 0.989, p < 0.001) before the reversal.
Conclusion
After two decades of decline, mortality involving both cardiomyopathy and liver disease rose sharply after 2018, especially among males and Native American and Black populations. This concerning trend may reflect increases in alcohol-related and metabolic liver disease, widening disparities in care, and pandemic-related disruptions. Targeted public health efforts are needed to address this dual burden and mitigate emerging cardiometabolic disparities.
More abstracts on this topic:
A Case of Clozapine-Induced Myocarditis: An Under-described Side Effect
Ibrahim Rand, Clearo Kellie
A Case of Hypertrophic Cardimyopathy: Digenic Variants of Uncertain Significance Mutations in MHY7 and RYR2 GenesDurukan Selina, Uzunoglu Ekin, Farahmandsadr Maryam, Soffer Daniel