Final ID: MP605
Impact of Prosthesis Deformation on Long-Term Outcomes After Balloon-Expandable Transcatheter Aortic Valve Replacement
Abstract Body (Do not enter title and authors here): Background: Transcatheter aortic valve replacement (TAVR) is a well-established therapy for severe aortic stenosis. However, suboptimal prosthesis deployment—such as under-expansion or geometric distortion—has emerged as a potential contributor to adverse clinical outcomes. While postprocedural computed tomography (CT) enables objective evaluation of valve geometry, its prognostic value in routine clinical practice remains unclear. In particular, the long-term clinical impact of prosthesis deformation following balloon-expandable TAVR has not been well characterized. We sought to evaluate the association between CT-defined prosthesis deformation and long-term outcomes in a contemporary real-world cohort.
Methods: We analyzed 1,221 patients from the RESOLVE registry who underwent balloon-expandable TAVR at Cedars-Sinai Medical Center between 2015 and 2022 and survived ≥30 days post-procedure. Clinical and procedural data were obtained from the STS/TVT registry. All patients underwent contrast-enhanced CT 30 days post-TAVR, with prosthesis geometry assessed by an independent CT core laboratory. Deformation was defined as under-expansion <90% and/or eccentricity ≥10% across all three valve levels (inflow, mid, and outflow). The primary outcome was a composite of all-cause mortality, stroke, or heart failure hospitalization.
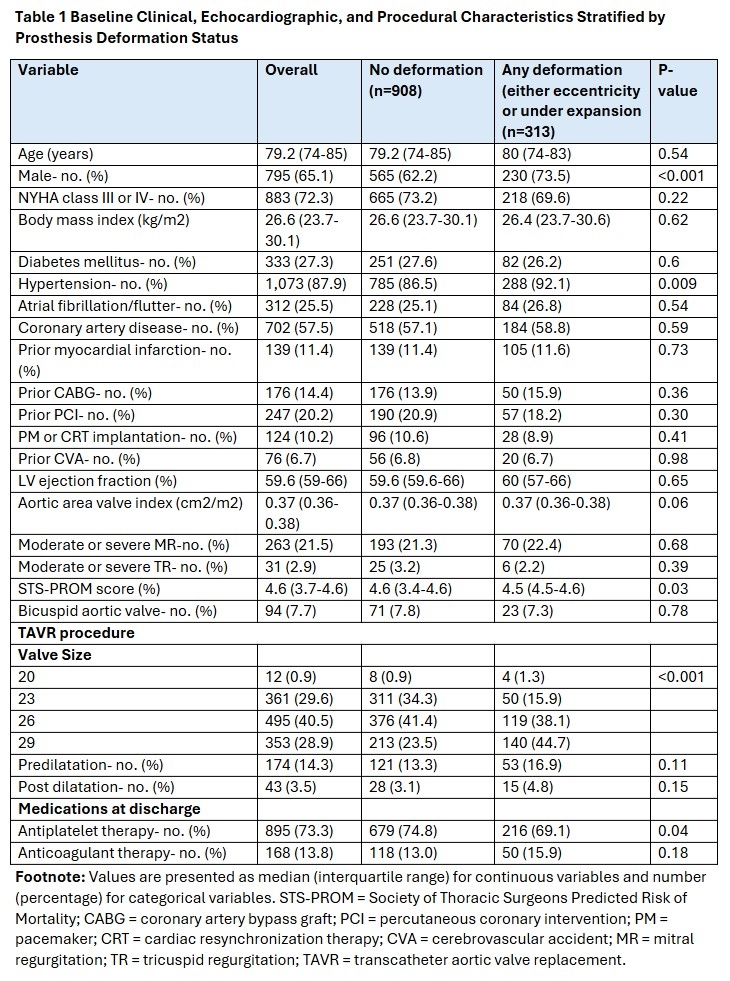
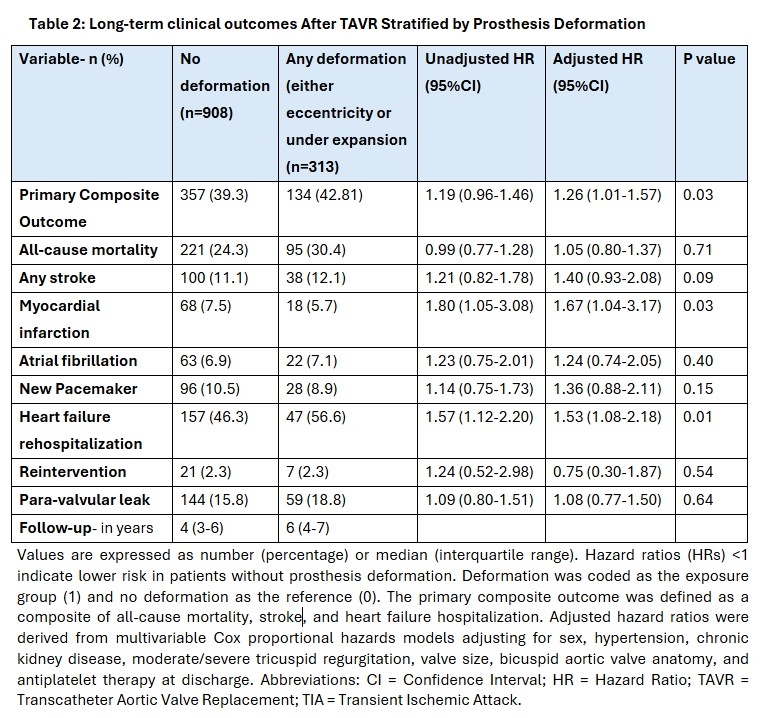
Results: Among the 1,221 patients, 313 (25.6%) exhibited prosthesis deformation. The overall cohort had a median follow-up of 5 years (IQR: 3–6). Baseline characteristics were generally comparable between groups, though deformation was more common in males (73.5% vs. 62.2%; p<0.001), those with hypertension (92.1% vs. 86.5%; p0.009), and recipients of a 29 mm valve (44.7% vs. 23.5%; p<0.001) (Table 1). The primary composite outcome was more frequent in the deformation group, with a significantly increased risk on Cox regression (HR 1.26; 95% CI 1.01–1.57; p0.03). Heart failure hospitalizations were also significantly higher. Although the absolute rate of myocardial infarction was lower, the adjusted risk was elevated. No significant differences were seen in all-cause mortality, stroke, new pacemaker implantation, or reintervention (Table 2).
Conclusion: In this high-volume TAVR cohort, prosthesis deformation was independently associated with worse long-term outcomes. These findings highlight the potential role of postprocedural CT imaging in identifying high-risk patients and informing strategies to optimize long-term outcomes following TAVR.
Methods: We analyzed 1,221 patients from the RESOLVE registry who underwent balloon-expandable TAVR at Cedars-Sinai Medical Center between 2015 and 2022 and survived ≥30 days post-procedure. Clinical and procedural data were obtained from the STS/TVT registry. All patients underwent contrast-enhanced CT 30 days post-TAVR, with prosthesis geometry assessed by an independent CT core laboratory. Deformation was defined as under-expansion <90% and/or eccentricity ≥10% across all three valve levels (inflow, mid, and outflow). The primary outcome was a composite of all-cause mortality, stroke, or heart failure hospitalization.
Results: Among the 1,221 patients, 313 (25.6%) exhibited prosthesis deformation. The overall cohort had a median follow-up of 5 years (IQR: 3–6). Baseline characteristics were generally comparable between groups, though deformation was more common in males (73.5% vs. 62.2%; p<0.001), those with hypertension (92.1% vs. 86.5%; p0.009), and recipients of a 29 mm valve (44.7% vs. 23.5%; p<0.001) (Table 1). The primary composite outcome was more frequent in the deformation group, with a significantly increased risk on Cox regression (HR 1.26; 95% CI 1.01–1.57; p0.03). Heart failure hospitalizations were also significantly higher. Although the absolute rate of myocardial infarction was lower, the adjusted risk was elevated. No significant differences were seen in all-cause mortality, stroke, new pacemaker implantation, or reintervention (Table 2).
Conclusion: In this high-volume TAVR cohort, prosthesis deformation was independently associated with worse long-term outcomes. These findings highlight the potential role of postprocedural CT imaging in identifying high-risk patients and informing strategies to optimize long-term outcomes following TAVR.
More abstracts on this topic:
Aortic Valve Calcification Density Performs Better Compared to Absolute Aortic Valve Calcification in Aortic Stenosis Risk Stratification
Ahmad Syed, Zeb Irfan, Watson Hangyu, Awad Maan, Patel Kunal, Nassar Sameh, Thyagaturu Harshith, Balla Sudarshan, Kawsara Mohammad, Daggubati Ramesh
A Case of Concomitant Wild-Type Transthyretin and Systemic Light Chain Amyloidosis Involving Separate OrgansChiu Leonard, Afrough Aimaz, Nadeem Urooba, Jebakumar Deborah, Grodin Justin