Final ID: MP268
Impact of Insurance Payor on ICU Length of Stay Among Stroke Patients: A Retrospective Cohort Study Using MIMIC-IV
Abstract Body (Do not enter title and authors here): Introduction: Insurance payor is an important social determinant of health that may serve as a proxy for socioeconomic status and mediate outcomes in healthcare. In 2010, 14 percent of stroke patients aged 19-64 lacked health insurance while stroke incidence in the United States continues to increase. Previous research has demonstrated that stroke patients with private insurance experience better clinical outcomes than those with public insurance and that Medicare is associated with longer hospital length of stay (LOS) than private insurance. However, no study has investigated the relationship between intensive care unit (ICU) LOS in stroke patients and insurance payor while controlling for stroke severity.
Research Question: Among ICU stroke patients, will those with private insurance have significantly longer ICU length of stay compared to patients with Medicare or Medicaid, after adjusting for demographics and stroke severity?
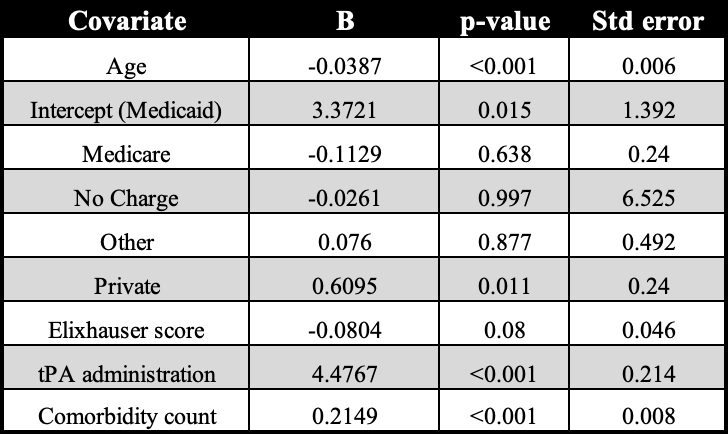
Method: We conducted a retrospective cohort study using the MIMIC-IV (v3.1) database to examine ICU LOS in days among adult stroke patients (≥18 years), identified by ICD-9 and ICD-10 codes for ischemic and hemorrhagic stroke. The primary independent variable was insurance payor (Medicare, Medicaid, Private, No Charge, Other). We adjusted for age, gender, race, comorbidity burden (Elixhauser score and ICD-based comorbidity count), and receipt of intravenous tPA as a proxy for stroke severity. Multivariable linear regression was used to assess the association between insurance status and ICU LOS.
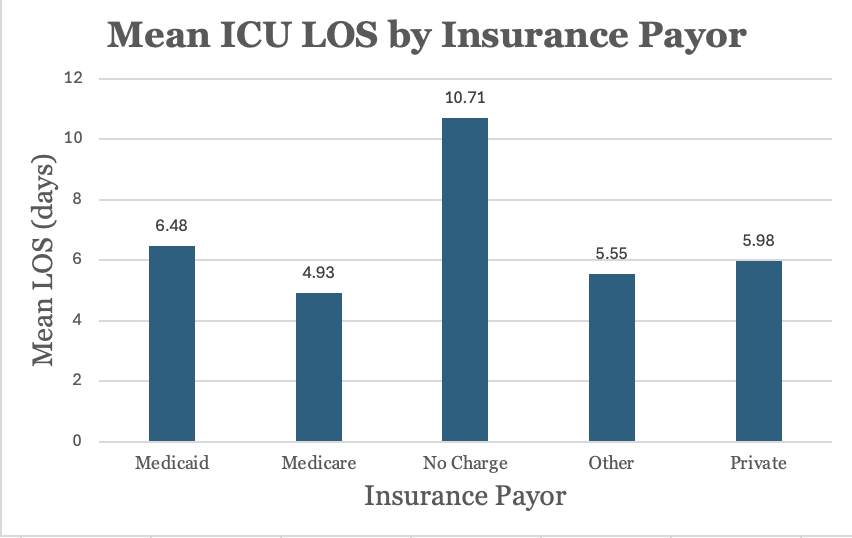
Results: A total of 9367 stroke ICU patients were included in the analysis. No Charge patients had the longest while Medicare patients had the shortest mean ICU LOS. Medicaid patients also had a longer mean ICU LOS than those privately insured. After controlling for stroke severity however, only private insurance was significantly associated with a longer ICU LOS compared to other insurance types. Other insurance payors did not show a significant association with ICU LOS.
Conclusion: Although privately insured stroke patients did not have the highest mean ICU LOS, private insurance was the only payor type significantly associated with increased ICU LOS after adjusting for demographics and stroke severity. These results suggest potential disparities in ICU resource allocation, post-acute care planning, discharge authorization, and reimbursement among insurance payors that warrant further investigation.
Research Question: Among ICU stroke patients, will those with private insurance have significantly longer ICU length of stay compared to patients with Medicare or Medicaid, after adjusting for demographics and stroke severity?
Method: We conducted a retrospective cohort study using the MIMIC-IV (v3.1) database to examine ICU LOS in days among adult stroke patients (≥18 years), identified by ICD-9 and ICD-10 codes for ischemic and hemorrhagic stroke. The primary independent variable was insurance payor (Medicare, Medicaid, Private, No Charge, Other). We adjusted for age, gender, race, comorbidity burden (Elixhauser score and ICD-based comorbidity count), and receipt of intravenous tPA as a proxy for stroke severity. Multivariable linear regression was used to assess the association between insurance status and ICU LOS.
Results: A total of 9367 stroke ICU patients were included in the analysis. No Charge patients had the longest while Medicare patients had the shortest mean ICU LOS. Medicaid patients also had a longer mean ICU LOS than those privately insured. After controlling for stroke severity however, only private insurance was significantly associated with a longer ICU LOS compared to other insurance types. Other insurance payors did not show a significant association with ICU LOS.
Conclusion: Although privately insured stroke patients did not have the highest mean ICU LOS, private insurance was the only payor type significantly associated with increased ICU LOS after adjusting for demographics and stroke severity. These results suggest potential disparities in ICU resource allocation, post-acute care planning, discharge authorization, and reimbursement among insurance payors that warrant further investigation.
More abstracts on this topic:
Area-Based Social Risk Measures and In-Hospital Mortality: A Comparative Modeling Study in Coronary Artery Disease Patients
Gao Zihang, Jiang Tian, Hong Haoyun, Thomas Kathie, Hall Jennifer, Zhao Juan
A Contactless and Automated Approach to the Acute Stroke AssessmentSaadat Moh, Titus Ryan, Verkuilen Haley, Fleming Phil, Sur Sanjib, Sen Souvik