Final ID: Sa3021
Optimizing Pediatric Cardiology Referrals: A Six-Year Quality Improvement Project from a UK District General Hospital
Abstract Body (Do not enter title and authors here): Background:
Paediatric cardiology referrals are increasing, placing pressure on district hospital services, with many not meeting criteria for specialist review. This QIP aimed to identify patterns of unnecessary referrals to guide triage and education.
Methods:
We retrospectively reviewed all first outpatient paediatric cardiology referrals between 2019 and 2024. Of 2,739 patients seen, 1,794 were new referrals. These were analysed by presenting complaint, referral source, and appropriateness based on national and local guidelines.
Results:
Of the 1,794 referrals, 910 (51%) were for murmurs, 178 (10%) for genetic syndromes, and 84 (5%) for definite cardiac conditions (e.g., Kawasaki disease, hypertension)—all appropriate.
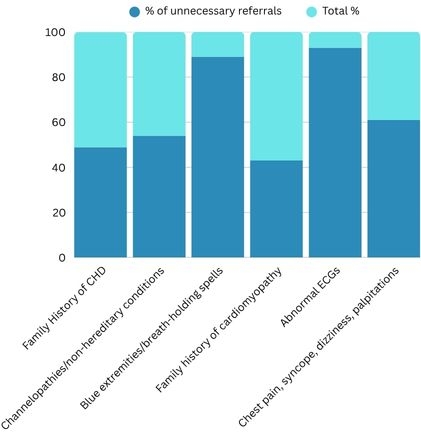
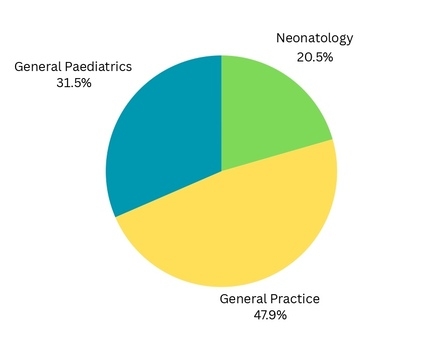
Inappropriate referrals were frequent. Of 135 family history referrals for congenital heart disease, 67 (50%) were appropriate, involving first-degree relatives with significant disease. The other 68 (50%) involved second- or third-degree relatives or non-heritable lesions (e.g., PDA, PFO), mostly from neonatal unit. Poor documentation contributed.
For cardiomyopathy history (n=44), 25 (57%) were appropriate, while 19 (43%) lacked clear inheritance patterns. Cyanosis or blue extremities (n=28) had only 3 (11%) appropriate referrals; the rest were likely acrocyanosis or Raynaud-type episodes. Only one child had a cardiac condition, already suspected by the presence of a murmur. Of 14 ECG abnormality referrals, only 1 was appropriate. Thirteen were normal but misread in general practice or general paediatrics. Channelopathy family history and non-heritable arrhythmias (n=39) included 17 (44%) appropriate and 22 (56%) inappropriate referrals, often involving distant relatives.
Among 362 referrals for chest pain, palpitations, or syncope, only 12 (3.3%) had cardiac pathology. Most symptoms (n=220, 61%) occurred predeominantly at rest. None of these cases had cardiac disease. One child diagnosed with extreme vasovagal syncope needed cardiac input, but general paediatrics could have arranged Holter monitoring before referral.
Conclusion:
Most of the cardiology referrals could have been reviewed in a general paediatric clinic thereby reducing the waiting times of the cardiac clinic. Targeted education, precise referral standards and guidance will enhance the triage process and ensure that the available cardiac clinic slots are utilized effectively. The impact of these interventions will have to be reassessed in a follow-up review.
Paediatric cardiology referrals are increasing, placing pressure on district hospital services, with many not meeting criteria for specialist review. This QIP aimed to identify patterns of unnecessary referrals to guide triage and education.
Methods:
We retrospectively reviewed all first outpatient paediatric cardiology referrals between 2019 and 2024. Of 2,739 patients seen, 1,794 were new referrals. These were analysed by presenting complaint, referral source, and appropriateness based on national and local guidelines.
Results:
Of the 1,794 referrals, 910 (51%) were for murmurs, 178 (10%) for genetic syndromes, and 84 (5%) for definite cardiac conditions (e.g., Kawasaki disease, hypertension)—all appropriate.
Inappropriate referrals were frequent. Of 135 family history referrals for congenital heart disease, 67 (50%) were appropriate, involving first-degree relatives with significant disease. The other 68 (50%) involved second- or third-degree relatives or non-heritable lesions (e.g., PDA, PFO), mostly from neonatal unit. Poor documentation contributed.
For cardiomyopathy history (n=44), 25 (57%) were appropriate, while 19 (43%) lacked clear inheritance patterns. Cyanosis or blue extremities (n=28) had only 3 (11%) appropriate referrals; the rest were likely acrocyanosis or Raynaud-type episodes. Only one child had a cardiac condition, already suspected by the presence of a murmur. Of 14 ECG abnormality referrals, only 1 was appropriate. Thirteen were normal but misread in general practice or general paediatrics. Channelopathy family history and non-heritable arrhythmias (n=39) included 17 (44%) appropriate and 22 (56%) inappropriate referrals, often involving distant relatives.
Among 362 referrals for chest pain, palpitations, or syncope, only 12 (3.3%) had cardiac pathology. Most symptoms (n=220, 61%) occurred predeominantly at rest. None of these cases had cardiac disease. One child diagnosed with extreme vasovagal syncope needed cardiac input, but general paediatrics could have arranged Holter monitoring before referral.
Conclusion:
Most of the cardiology referrals could have been reviewed in a general paediatric clinic thereby reducing the waiting times of the cardiac clinic. Targeted education, precise referral standards and guidance will enhance the triage process and ensure that the available cardiac clinic slots are utilized effectively. The impact of these interventions will have to be reassessed in a follow-up review.
More abstracts on this topic:
A Multicenter Friedreich Ataxia Registry Identifies Posterior Wall Thickness as a Predictor of Major Adverse Cardiac Events
Lin Kimberly, Johnson Jonathan, Mccormack Shana, Lynch David, Tate Barbara, Feng Yixuan, Huang Jing, Mercer-rosa Laura, Dedio Anna, Mcsweeney Kara, Fournier Anne, Yoon Grace, Payne Ronald, Cripe Linda, Patel Aarti, Niaz Talha
Applying a comprehensive cardiometabolic risk prediction model to real-world primary care patient dataHowell Carrie, Tanaka Shiori, Burkholder Greer, Mehta Tapan, Herald Larry, Garvey William, Cherrington Andrea