Final ID: Su3039
Echocardiographic Variables Associated with Postnatal Compromise and Mortality in Prenatally Diagnosed Tetralogy of Fallot with Absent Pulmonary Valve, a Fetal Heart Society Collaborative Study
Research Questions: To evaluate the relationship between prenatal and postnatal echocardiographic measures and whether postnatal echocardiographic findings were associated with morbidity and mortality.
Methods: We included liveborn patients from the prenatally diagnosed multicenter cohort. Differences between prenatal and postnatal measures were assessed using the paired t-test. Association between postnatal echocardiographic measures and outcomes were assessed using logistic regression. Outcomes included respiratory arrest, inotrope use, cardiac arrest, extracorporeal membrane oxygenation within 48 hours of birth, surgery during initial admission, death prior to and after discharge.
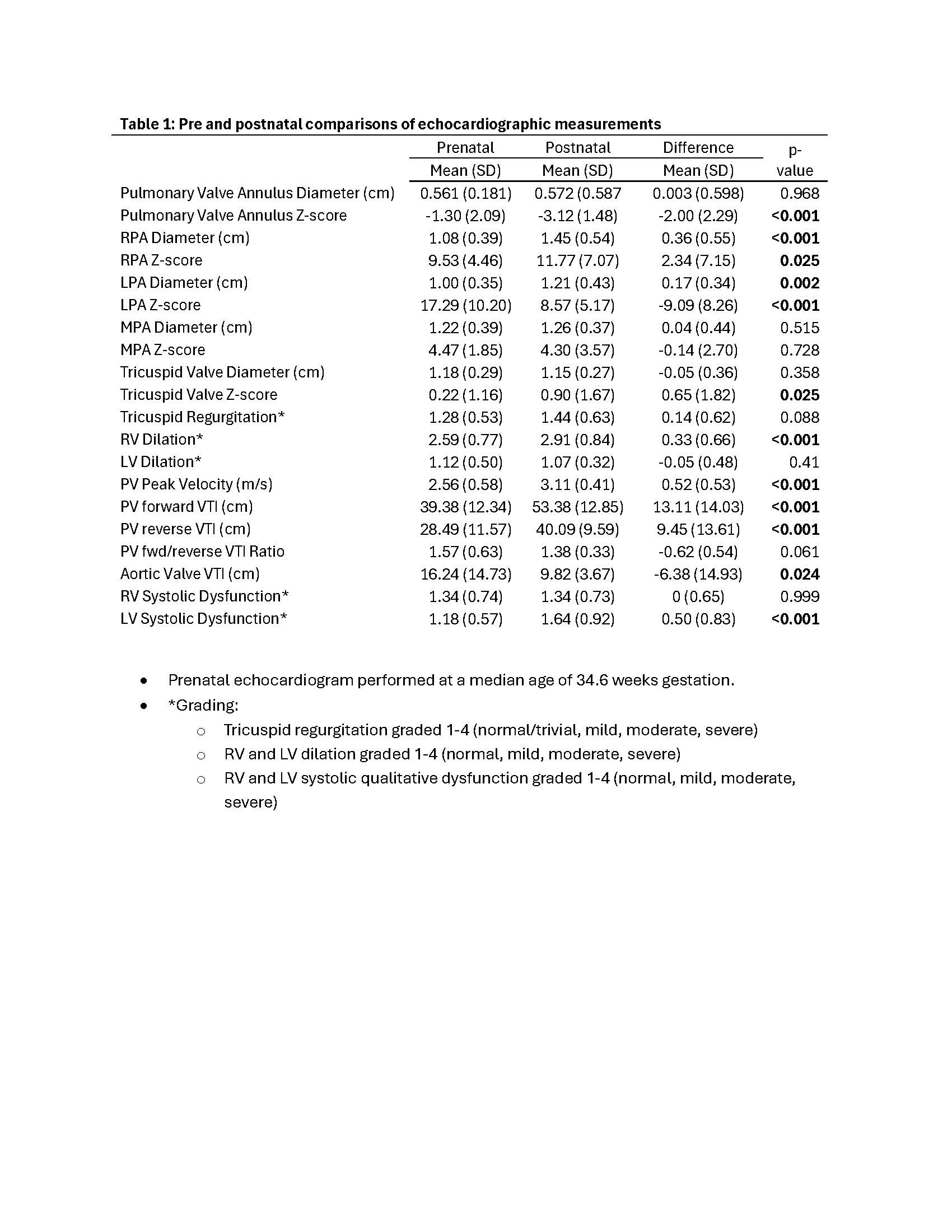
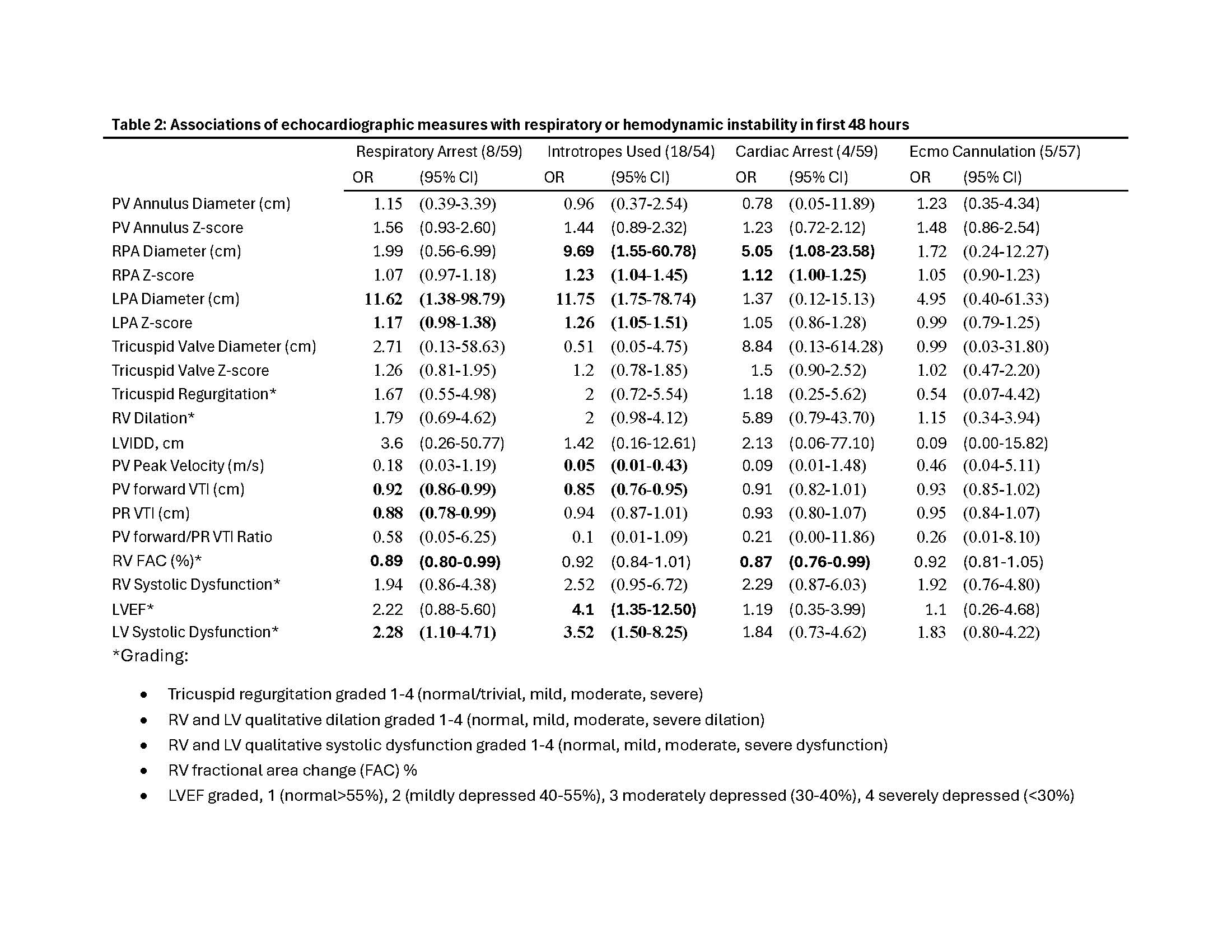
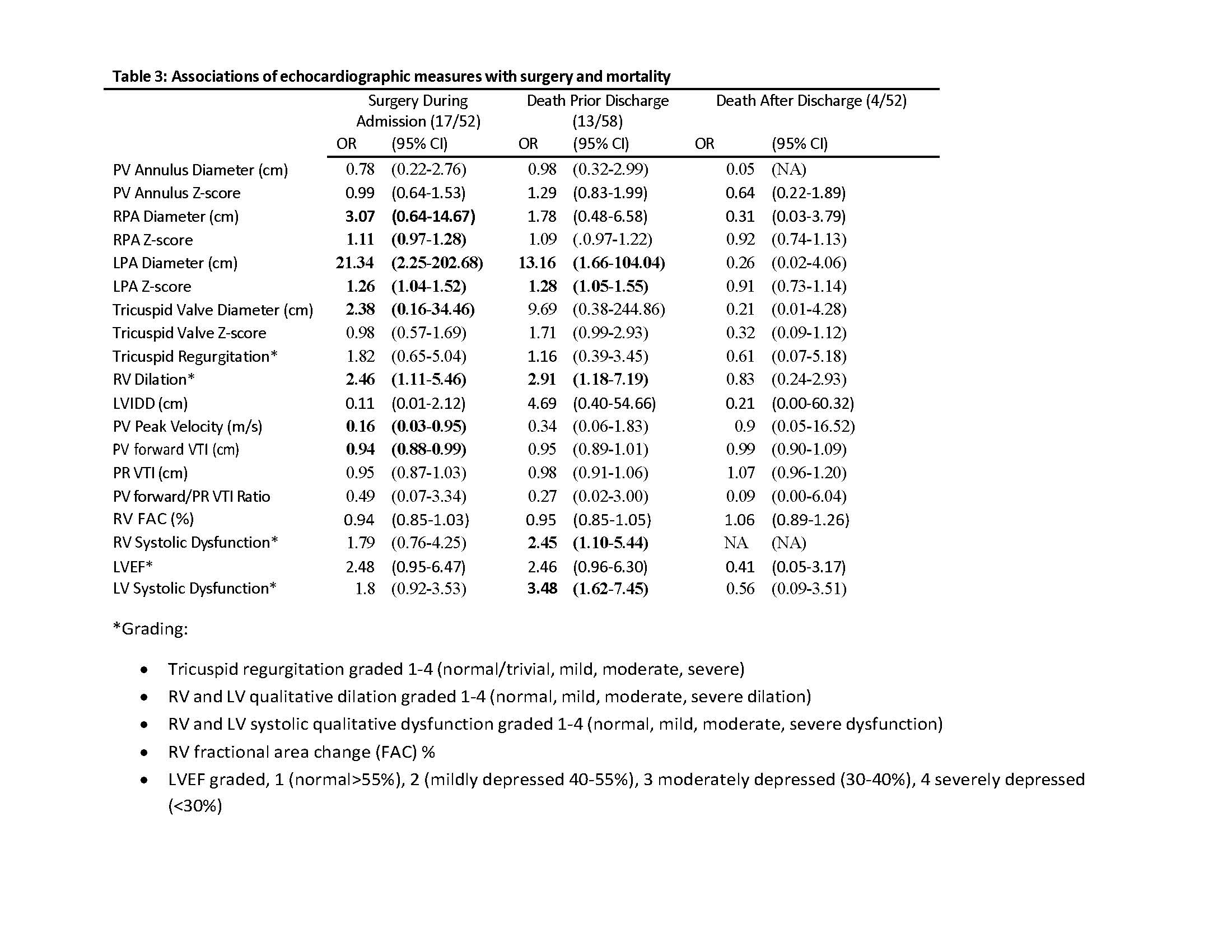
Results: Of 59 patients (42% male), mean gestational age at birth was 37.9 weeks and birthweight 2877 grams. Abnormal genetics were present in 23/53 (39%), with 20/53 (34%) with 22q11 deletion. Postnatal echo had larger branch PA diameters and RV size with increased pulmonary valve (PV) peak velocity and velocity time integral (VTI) and decreased LV function (Table 1). Univariate analysis revealed RV systolic dysfunction to be associated with respiratory and cardiac arrest. LV systolic dysfunction was associated with inotrope use and respiratory arrest (Table 2). Higher PV peak velocity and PV VTI were associated with lower likelihood of inotrope use, respiratory arrest, and surgery during initial admission. RV dilation, RV and LV systolic dysfunction were associated with death prior to discharge. Increased branch PA diameter correlated with respiratory arrest, inotrope use, early surgery, and death prior to discharge (Table 2,3).
Conclusions: Signs of poor cardiac output including increased RV dilation and RV or LV dysfunction were associated with poor outcome. Newborns with increased PV peak velocity and VTI after birth had better outcomes, possibly due to better RV systolic function or decreased pulmonary vascular resistance (anatomical or functional). In contrast to prenatal findings, larger branch PA diameter was associated with poor outcome.
- Udine, Michelle ( Children's National Hospital , Washington , District of Columbia , United States )
- Carroll, Sheila ( Weill Cornell Medicine , New York , New York , United States )
- Hogan, Whitnee ( University of Utah , Salt Lake City , Utah , United States )
- Levasseur, Stephanie ( Columbia University , New York , New York , United States )
- Howley, Lisa ( Children's Minnesota , Plymouth , Minnesota , United States )
- Chiu, Joanne ( Mass General Hospital , Boston , Massachusetts , United States )
- Hornberger, Lisa ( UNIV ALBERTA , Edmonton , Alberta , Canada )
- Moon-grady, Anita ( Univ. of California San Francisco , San Francisco , California , United States )
- Cohen, Jennifer ( Mount Sinai , Merrick , New York , United States )
- Arya, Bhawna ( SEATTLE CHILDREN'S HEART CENTER , Seattle , Washington , United States )
- Peyvandi, Shabnam ( UNIVERSITY CALIFORNIA SAN FRAN , San Francisco , California , United States )
- Barber, John ( Children's National Hospital , Washington , District of Columbia , United States )
- Morris, Shaine ( Texas Children's Hospital , Houston , Texas , United States )
- Chelliah, Anjali ( Atlantic Medical Group , Morristown , New Jersey , United States )
- Donofrio, Mary ( Childrens National Medical Center , Washington , District of Columbia , United States )
- Divanovic, Allison ( CINCINNATI CHILDRENS HOSPITAL , Cincinnati , Ohio , United States )
- Kovalchin, John ( NATIONWIDE CHILDRENS HOSP , Columbus , Ohio , United States )
- Lindblade, Chris ( Phoenix Children's Hospital , Phoenix , Arizona , United States )
- Pruetz, Jay ( Cedars Sinai , Los Angeles , California , United States )
- Schidlow, David ( Boston Children's Hospital , Boston , Massachusetts , United States )
- Yeh, Jay ( UC Davis , Oakland , California , United States )
- Zoeller, Bridget ( LURIE CHILDRENS HOSPITAL , Chicago , Illinois , United States )
Meeting Info:
Session Info:
Potpourri 1: Pediatric and Congenital Cardiology
Sunday, 11/09/2025 , 11:30AM - 12:30PM
Abstract Poster Board Session
More abstracts on this topic:
Ali Manzer, Umar Haddaya, Nazir Tahira, Nizam Muhammad, Steafo Lark, Sharif Ayesha, Jehangir Hanzala, Arham Muhammad, Hamza Anfal, Hassan Arbaz, Amjad Ans, Ali Iman, Zuha Zuha
A Novel Echocardiography Risk Score Predicted Mortality In Patients With Heart Failure With Preserved Ejection Fraction.Iwakura Katsuomi, Yoshio Yasumura, Hikoso Shungo, Okada Katsuki, Nakatani Daisaku, Sotomi Yohei, Sakata Yasushi, Tanaka Nobuaki, Okada Masato, Okamura Atsunori, Heitaro Watanabe, Seo Masahiro, Hayashi Takaharu, Yano Masamichi, Yamada Takahisa
More abstracts from these authors:
Keller Sam, Moon-grady Anita, Peyvandi Shabnam, Ronai Christina, Taylor Carolyn, Thakur Varsha, Zinis Sofia, Morris Shaine, Barris David, Cohen Jennifer, Gonsalves Clarelle, Hogan Whitnee, Hornberger Lisa, Howley Lisa, Krishnan Anita, Mcbrien Angela
Outcomes of Hypoplastic Left Heart Syndrome by Subtype and Presence of Ventriculocoronary Connections: A Fetal Heart Society Multi-Center Retrospective studyBarris David, Moon-grady Anita, Michelfelder Erik, Mcbrien Angela, Hornberger Lisa, Lee Caroline, Hogan Whitnee, Chelliah Anjali, Howley Lisa, Arya Bhawna, Keller Sam, Freud Lindsay, Krishnan Anita, Donofrio Mary, Taylor Carolyn, Husain Nazia, Lemley Bethan, Ronai Christina, Tworetzky Wayne, Ikemba Catherine, Gonsalves Clarelle, Geiger Miwa, Day Patrick, Duong Son, Cohen Jennifer, Morris Shaine, Lopez Keila, Kavanaugh-mchugh Ann, Killen Stacy, Peyvandi Shabnam, Nunez Gallegos Flora