Final ID: Mo1016
Congestion Limits Reduction in Left Ventricular Pressure-Volume Area Due to Veno-Arterial Extracorporeal Membrane Oxygenation (VA-ECMO) in Acute Myocardial Infarction
Abstract Body (Do not enter title and authors here): Background: Use of veno-arterial extracorporeal membrane oxygenation (VA-ECMO) is increasing in acute myocardial infarction (AMI) and heart failure associated cardiogenic shock. We previously reported that in AMI VA-ECMO can reduce left-ventricular (LV) pressure-volume area (PVA), a key correlate of myocardial oxygen consumption. However, whether these findings extend to states of congestion is unknown.
Hypothesis: We hypothesized that congestion limits the ability of VA-ECMO to reduce biventricular volumes (preload) and pressure-volume area in AMI.
Methods: Large swine underwent ischemia-reperfusion injury (IRI) via mid-left anterior descending (LAD) artery occlusion for 60 minutes followed by 180 minutes of reperfusion (n=6 per group). In the congested arm, prior to LAD occlusion, animals received IV fluid until right atrial pressure (RAP) exceeded 12 mmHg. After 30 minutes of reperfusion, VA-ECMO was activated in both groups. Invasive arterial, venous, and biventricular pressure-volume measurements and echocardiograms were obtained.
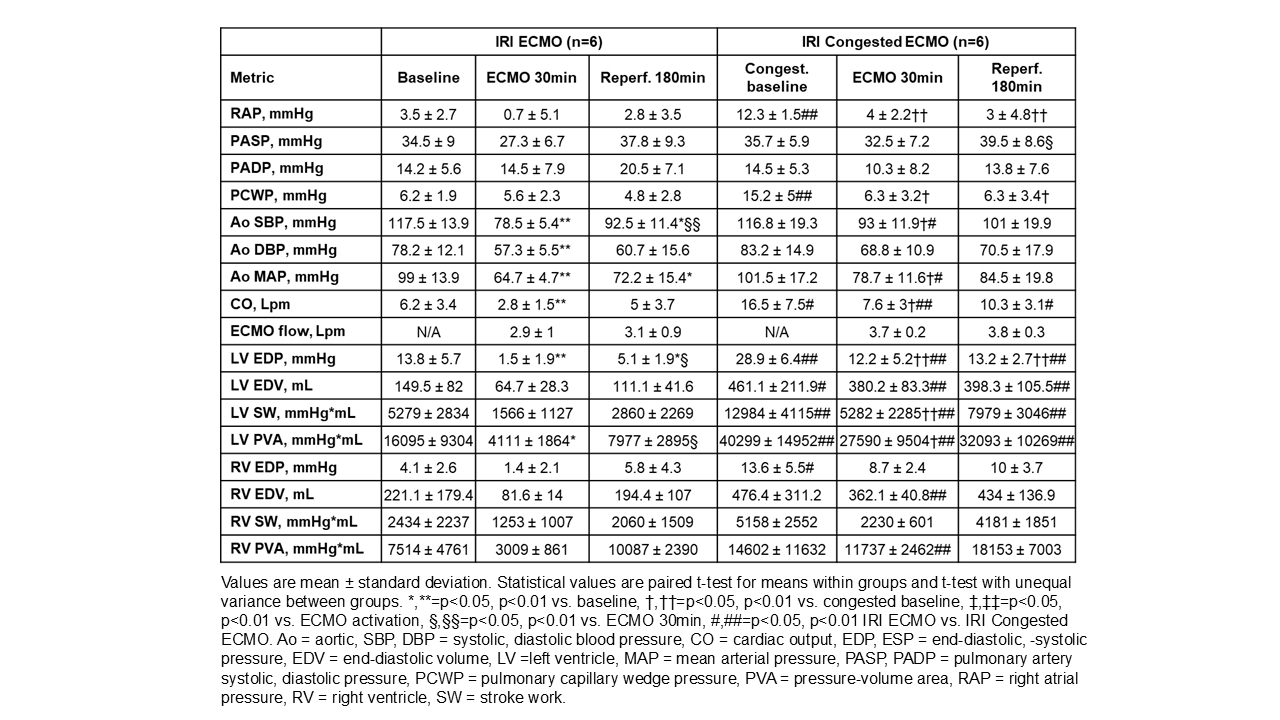
Results: Prior to IRI, congested animals had higher RAP, right-ventricular (RV) end-diastolic pressure (EDP), pulmonary capillary wedge pressure (PCWP), LV EDP, LV end-diastolic volume (EDV), cardiac output (CO), LV stroke work (SW) and LV PVA than noncongested animals (Table 1). Acutely after VA-ECMO activation, congested animals had an increase in LV PVA which was not observed in the noncongested group. After 30 minutes of VA-ECMO, both groups had a reduction in LV EDP, CO, aortic mean and systolic blood pressures and LV PVA, compared to baseline. However, at both 30 minutes of VA-ECMO and 180 minutes of reperfusion, LV PVA was higher in the congested group (Fig. 1A). After 30 minutes of ECMO, RV PVA was lower in the noncongested group (Fig. 1B).
Conclusion: We report for the first time that VA-ECMO associated reductions in biventricular pressure-volume area may be limited in states of congestion. Future studies testing whether reducing total cardiac preload with drugs and/or devices in VA-ECMO minimizes ventricular load are required.
Hypothesis: We hypothesized that congestion limits the ability of VA-ECMO to reduce biventricular volumes (preload) and pressure-volume area in AMI.
Methods: Large swine underwent ischemia-reperfusion injury (IRI) via mid-left anterior descending (LAD) artery occlusion for 60 minutes followed by 180 minutes of reperfusion (n=6 per group). In the congested arm, prior to LAD occlusion, animals received IV fluid until right atrial pressure (RAP) exceeded 12 mmHg. After 30 minutes of reperfusion, VA-ECMO was activated in both groups. Invasive arterial, venous, and biventricular pressure-volume measurements and echocardiograms were obtained.
Results: Prior to IRI, congested animals had higher RAP, right-ventricular (RV) end-diastolic pressure (EDP), pulmonary capillary wedge pressure (PCWP), LV EDP, LV end-diastolic volume (EDV), cardiac output (CO), LV stroke work (SW) and LV PVA than noncongested animals (Table 1). Acutely after VA-ECMO activation, congested animals had an increase in LV PVA which was not observed in the noncongested group. After 30 minutes of VA-ECMO, both groups had a reduction in LV EDP, CO, aortic mean and systolic blood pressures and LV PVA, compared to baseline. However, at both 30 minutes of VA-ECMO and 180 minutes of reperfusion, LV PVA was higher in the congested group (Fig. 1A). After 30 minutes of ECMO, RV PVA was lower in the noncongested group (Fig. 1B).
Conclusion: We report for the first time that VA-ECMO associated reductions in biventricular pressure-volume area may be limited in states of congestion. Future studies testing whether reducing total cardiac preload with drugs and/or devices in VA-ECMO minimizes ventricular load are required.
More abstracts on this topic:
A New Analytical Approach for Noninvasive Reconstruction of the Entire Left Ventricular Pressure Waveform in Myocardial Ischemia and Infarction
Bilgi Coskun, Li Jiajun, Alavi Rashid, Dai Wangde, Matthews Ray, Kloner Robert, Pahlevan Niema
A First-in-Class Humanized Antibody Fragment Targeting Platelet Glycoprotein Ibα: A Comprehensive Preclinical Study of CA1001 for the Treatment of Acute Ischemic StrokeXu Xiaohong, Preeti Preeti, Yu Ruoying, Shaykhalishahi Hamed, Zhang Cheng, Shen Chuanbin, Li Bei, Tang Naping, Chang Yan, Xiang Qian, Cui Yimin, Lei Xi, Ni Heyu, Zhu Guangheng, Liu Zhenze, Hu Xudong, Slavkovic Sladjana, Neves Miguel, Ma Wenjing, Xie Huifang