Final ID: MP760
Primary Graft Dysfunction in Pediatric Transplant: Insights from the Organ Procurement and Transplantation Network
Abstract Body (Do not enter title and authors here): Introduction: We describe the incidence of primary graft dysfunction (PGD) in the pediatric heart transplant population. This has been difficult to quantify because of uncertain definitions and the lack of an encompassing database leading to the use of surrogates such as the need for mechanical circulatory support in the 24-48 hours post-transplant. Since September 2023 the OPTN database has included PGD and we provide an interim analysis of PGD including its incidence and relationship to mortality.
Methods: The United Network for Organ Sharing database was queried for pediatric patients (<18 years) who received a heart transplant in the United States and had data pertaining to PGD at 24 hours post-transplantation. Univariable analysis was performed to assess baseline, perioperative, and post-operative characteristics, employing chi-square analysis and student's Wilcoxon rank sum tests. Post-transplant survival was compared using Kaplan-Meier analysis with a log-rank test.
Results: A total of 656 patients were included in the final cohort, of whom 11.2% (N=77) had PGD at 24 hours. Patients with PGD were significantly younger than those without PGD (median age 7.1 years [IQR: 1–14] vs. 8.9 years [IQR: 2–15], p = 0.016). The groups were similar in weight (27.1 kg [IQR: 7.3–39.5] vs. 26.2 kg [IQR: 10.0–50.0] and rates of congenital heart disease (CHD) (58.4% [N=45] vs. 55.1% [N=318], p = 0.667).
Pretransplant VAD support was similar between groups (50.6% [N=39] vs. 41.8% [N=241], p = 0.175), as were the rates of Berlin Heart EXCOR utilization and LVSD configuration.
Among the 77 patients with PGD at 24 hours, 41 (53.2%) continued to have PGD at 72 hours. Patients with PGD at 72 hours experienced significantly higher rates of postoperative stroke (17.3% [N=13/75] vs. 3.3% [N=19/574], p < 0.001) and dialysis (29.9% [N=23] vs. 5.9% [N=34/576], p < 0.001).
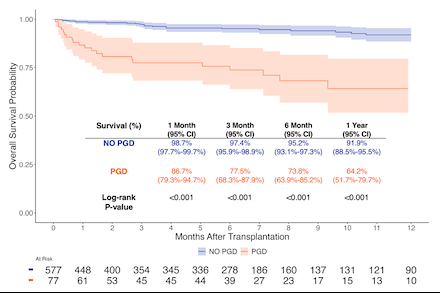
Kaplan-Meier survival analysis showed that patients with PGD at 24 hours had significantly worse survival at 1 month (86.7% [95% CI: 79.3%–94.7%] vs. 98.7% [95% CI: 95.9%–98.9%]) and 1 year (64.2% [95% CI: 51.7%–79.7%] vs. 91.9% [95% CI: 88.5%–95.5%]) compared to those without PGD (log-rank p < 0.001 for all; Figure 1).
Conclusion: The incidence of PGD in this contemporary cohort is more than two times that of previously reported studies and is associated with significantly increased mortality. The inclusion of PGD in the OPTN database will allow a more extensive characterization of this entity in the future.
Methods: The United Network for Organ Sharing database was queried for pediatric patients (<18 years) who received a heart transplant in the United States and had data pertaining to PGD at 24 hours post-transplantation. Univariable analysis was performed to assess baseline, perioperative, and post-operative characteristics, employing chi-square analysis and student's Wilcoxon rank sum tests. Post-transplant survival was compared using Kaplan-Meier analysis with a log-rank test.
Results: A total of 656 patients were included in the final cohort, of whom 11.2% (N=77) had PGD at 24 hours. Patients with PGD were significantly younger than those without PGD (median age 7.1 years [IQR: 1–14] vs. 8.9 years [IQR: 2–15], p = 0.016). The groups were similar in weight (27.1 kg [IQR: 7.3–39.5] vs. 26.2 kg [IQR: 10.0–50.0] and rates of congenital heart disease (CHD) (58.4% [N=45] vs. 55.1% [N=318], p = 0.667).
Pretransplant VAD support was similar between groups (50.6% [N=39] vs. 41.8% [N=241], p = 0.175), as were the rates of Berlin Heart EXCOR utilization and LVSD configuration.
Among the 77 patients with PGD at 24 hours, 41 (53.2%) continued to have PGD at 72 hours. Patients with PGD at 72 hours experienced significantly higher rates of postoperative stroke (17.3% [N=13/75] vs. 3.3% [N=19/574], p < 0.001) and dialysis (29.9% [N=23] vs. 5.9% [N=34/576], p < 0.001).
Kaplan-Meier survival analysis showed that patients with PGD at 24 hours had significantly worse survival at 1 month (86.7% [95% CI: 79.3%–94.7%] vs. 98.7% [95% CI: 95.9%–98.9%]) and 1 year (64.2% [95% CI: 51.7%–79.7%] vs. 91.9% [95% CI: 88.5%–95.5%]) compared to those without PGD (log-rank p < 0.001 for all; Figure 1).
Conclusion: The incidence of PGD in this contemporary cohort is more than two times that of previously reported studies and is associated with significantly increased mortality. The inclusion of PGD in the OPTN database will allow a more extensive characterization of this entity in the future.
More abstracts on this topic:
Acceptability and Gain of Knowledge of Community Educational Tools About Rheumatic Heart Disease Integrated With Screening In Low-Income Settings
Abrams Jessica, Nunes Maria, Diniz Marina, Fraga Lucas, Paula Luiza, Coelho Cecilia, Tacuri Chavez Luz Marina, Lemos Larissa, Correia Julliane, Ribeiro Antonio, Nascimento Bruno, Sable Craig, Spaziani Alison, Zuhlke Liesl, Cardoso Clareci, Vinhal Wanessa, Ribeiro Isabely, Oliveira Kaciane, Amaral Ingred Beatriz
Agbaje’s Waist-to-Height Ratio Estimated Fat Mass Pediatric Cutoff Predicts Elevated Blood Pressure Risk in Multi-racial US Children and AdolescentsCorsi Douglas, Agbaje Andrew