Final ID: MP1972
Discontinuation of Beta-Blockers After Acute Coronary Syndrome: A Systematic Review and Meta-Analysis
Abstract Body (Do not enter title and authors here):
Introduction: The optimal duration of beta-blocker (BB) therapy after myocardial infarction remains uncertain in patients without heart failure, especially given their frequent lifelong use and potential adverse effects.
Research Question: To address this gap, we conducted a meta-analysis to evaluate the impact of BB discontinuation on clinical outcomes in patients with preserved left ventricular ejection fraction (LVEF).
Methods: PubMed, Embase, and the Cochrane Central Register of Controlled Trials were systematically searched for studies enrolling patients with acute coronary syndrome (ACS) and preserved LVEF (≥50%), comparing BB discontinuation versus continuation. Outcomes of interest included all-cause mortality (ACM), major adverse cardiovascular events (MACE), cardiovascular (CV) death, non-CV death, cardiovascular hospitalisation, myocardial infarction, stroke, and unplanned revascularisation. Risk ratios (RR) and hazard ratios (HR) were pooled using random-effects models with 95% confidence intervals (CI). Statistical significance was defined as p < 0.05, and analyses were conducted using RStudio.
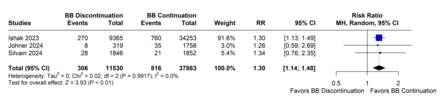
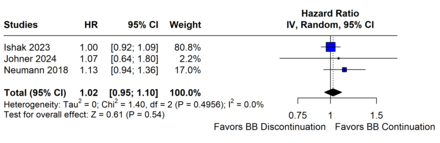
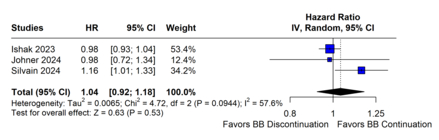
Results: Six studies, including 144,661 patients, were analysed. The mean age ranged from 57 to 65 years. In four studies, BB were discontinued after 12 months, while in the remaining two, discontinuation occurred at 11 and 6 months, respectively. The prevalence of hypertension ranged from 23.8% to 42.6%. BB discontinuation was associated with increased risk of CV death (RR 1.30; 95% CI 1.14–1.48; p < 0.01; Figure 1A), non-CV death (RR 1.16; 95% CI 1.07–1.25; p < 0.01), and myocardial infarction (RR 1.11; 95% CI 1.03–1.19; p < 0.01; Figure 1B). However, when accounting for time-to-event data, there were no significant differences in ACM (HR 1.02; 95% CI 0.95–1.10; p = 0.54; Figure 1C) or MACE (HR 1.04; 95% CI 0.92–1.18; p = 0.53; Figure 1D). No differences were observed for stroke (HR 1.02; 95% CI 0.89–1.17; p = 0.74) or unplanned revascularisation (RR 0.95; 95% CI 0.86–1.06; p = 0.74).
Conclusion: In this meta-analysis, discontinuing BB after ACS in patients with preserved LVEF was associated with higher risks of CV and non-CV death, as well as myocardial infarction. No differences were found in ACM or MACE. These results underscore the need for further studies to identify patient subgroups that may benefit most from continued therapy.
Introduction: The optimal duration of beta-blocker (BB) therapy after myocardial infarction remains uncertain in patients without heart failure, especially given their frequent lifelong use and potential adverse effects.
Research Question: To address this gap, we conducted a meta-analysis to evaluate the impact of BB discontinuation on clinical outcomes in patients with preserved left ventricular ejection fraction (LVEF).
Methods: PubMed, Embase, and the Cochrane Central Register of Controlled Trials were systematically searched for studies enrolling patients with acute coronary syndrome (ACS) and preserved LVEF (≥50%), comparing BB discontinuation versus continuation. Outcomes of interest included all-cause mortality (ACM), major adverse cardiovascular events (MACE), cardiovascular (CV) death, non-CV death, cardiovascular hospitalisation, myocardial infarction, stroke, and unplanned revascularisation. Risk ratios (RR) and hazard ratios (HR) were pooled using random-effects models with 95% confidence intervals (CI). Statistical significance was defined as p < 0.05, and analyses were conducted using RStudio.
Results: Six studies, including 144,661 patients, were analysed. The mean age ranged from 57 to 65 years. In four studies, BB were discontinued after 12 months, while in the remaining two, discontinuation occurred at 11 and 6 months, respectively. The prevalence of hypertension ranged from 23.8% to 42.6%. BB discontinuation was associated with increased risk of CV death (RR 1.30; 95% CI 1.14–1.48; p < 0.01; Figure 1A), non-CV death (RR 1.16; 95% CI 1.07–1.25; p < 0.01), and myocardial infarction (RR 1.11; 95% CI 1.03–1.19; p < 0.01; Figure 1B). However, when accounting for time-to-event data, there were no significant differences in ACM (HR 1.02; 95% CI 0.95–1.10; p = 0.54; Figure 1C) or MACE (HR 1.04; 95% CI 0.92–1.18; p = 0.53; Figure 1D). No differences were observed for stroke (HR 1.02; 95% CI 0.89–1.17; p = 0.74) or unplanned revascularisation (RR 0.95; 95% CI 0.86–1.06; p = 0.74).
Conclusion: In this meta-analysis, discontinuing BB after ACS in patients with preserved LVEF was associated with higher risks of CV and non-CV death, as well as myocardial infarction. No differences were found in ACM or MACE. These results underscore the need for further studies to identify patient subgroups that may benefit most from continued therapy.
More abstracts on this topic:
Cardiac projecting NPY2r expressing neurons in stellate ganglia remodel myocardium in cardiac injury-related settings
Sharma Sachin
β-1 Adrenoceptor is Responsible for the Apamin-Sensitive Small Conductance Ca2+-Activated K+ Current Activation in Female Rabbit VentriclesYang Minjing, Zhang Liyang, Kote Anxhela, Tisdale James, Chen Zhenhui, Everett Thomas, Chen Peng-sheng, Liu Xiao