Final ID: Su3077
Impact of Hemophilia on In-Hospital Outcomes Among Patients Undergoing Coronary Artery Bypass Graft: A Propensity-Matched Analysis of the National Inpatient Sample (2016–2022)
Abstract Body (Do not enter title and authors here): Introduction
Hemophilia is a rare bleeding disorder characterized by deficient clotting factors, which may increase perioperative risks in patients undergoing major cardiac surgery such as coronary artery bypass grafting (CABG). Data on in-hospital outcomes of hemophilic patients undergoing CABG remain scarce.
Hypothesis
We hypothesized that patients with hemophilia undergoing CABG experience worse in-hospital outcomes compared to their non-hemophilic counterparts.
Objectives
To evaluate the impact of hemophilia on in-hospital mortality, length of stay (LOS), and hospitalization costs in patients undergoing CABG.
Methods
We conducted a retrospective cohort study using the National Inpatient Sample (NIS) from 2016 to 2022. Adult patients undergoing CABG were identified using validated ICD-10-PCS codes. Patients with a diagnosis of hemophilia were matched to non-hemophilic patients using 4:1 propensity score matching (PSM) based on sociodemographic and clinical characteristics. Covariate balance was assessed using standardized mean differences. Conditional logistic regression was used to calculate odds ratios for in-hospital mortality, generalized linear models with a gamma distribution and a log-link function were used to evaluate differences in LOS and hospitalization costs.
Results
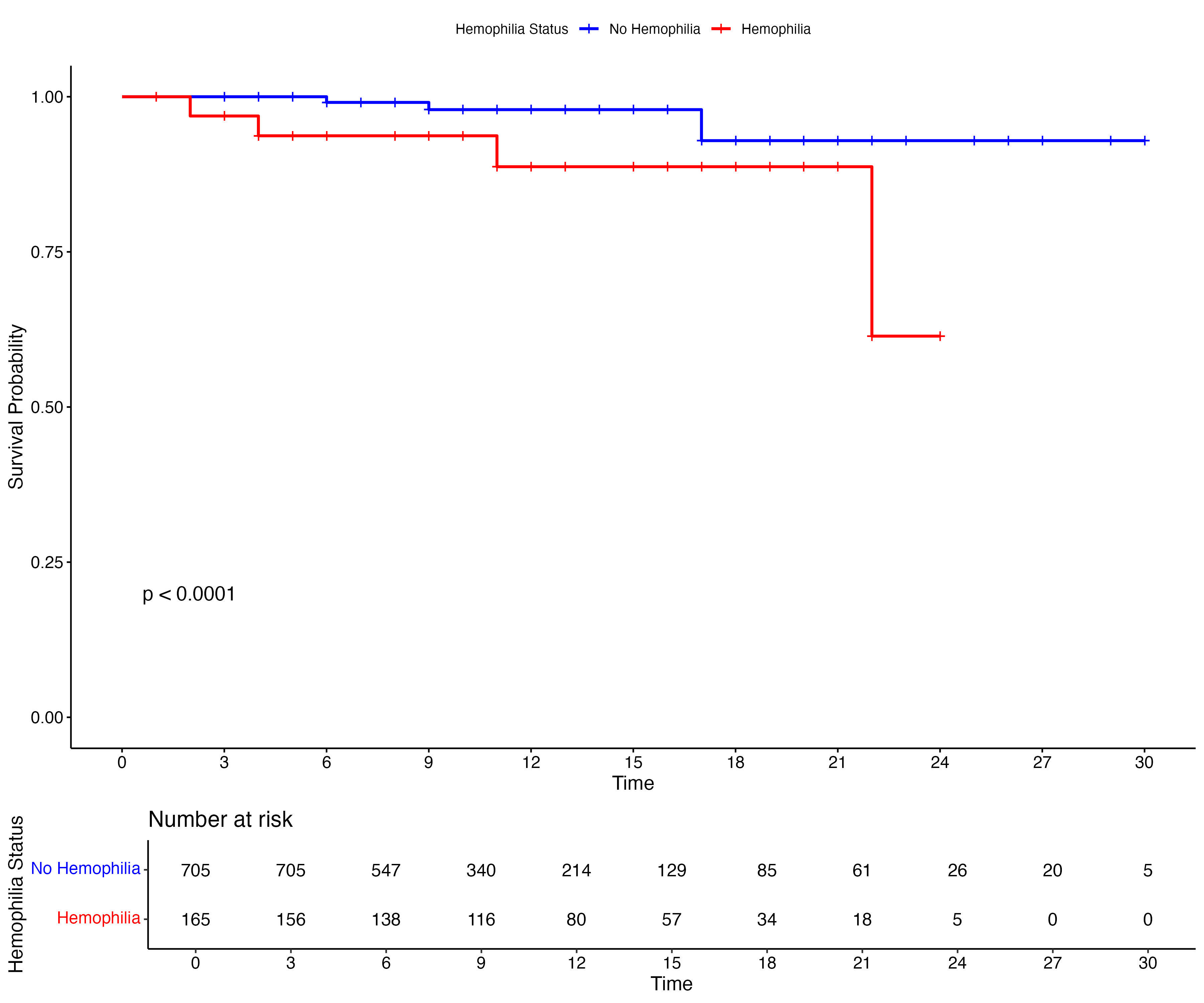
A weighted total of 280 hospitalizations for coronary artery bypass grafting (CABG) among patients with hemophilia were identified. Following 4:1 PSM, the final cohort comprised 900 patients—180 with hemophilia and 720 without. The mean age was 63.2 years (SD 10.6), and 74.7% of patients were White. Hemophilia A accounted for 58.3% of the hemophilia patients, while Hemophilia B & C accounted for 14.4% and 27.3%, respectively. The overall in-hospital mortality rate was 4.2%. Mortality was significantly higher in the hemophilic group (10.6%) compared to the non-hemophilic group (2.6%) (OR: 4.5 (95% CI: 2.4–6.4). The median length of stay (LOS) for the entire cohort was 9 days (IQR: 8 days), and the median hospitalization cost was $46,440 (IQR: $42,654). Compared to non-hemophilic patients, those with hemophilia had a 33% longer LOS (β = 1.33 days; 95% CI: 1.18–1.49) and 62% higher hospitalization costs (β = 1.62; 95% CI: 1.43–1.84).
Conclusion
Hemophilia is linked to higher in-hospital mortality, longer stays, and greater costs in patients undergoing CABG. These findings highlight the need for enhanced perioperative care and tailored management in this high-risk group.
Hemophilia is a rare bleeding disorder characterized by deficient clotting factors, which may increase perioperative risks in patients undergoing major cardiac surgery such as coronary artery bypass grafting (CABG). Data on in-hospital outcomes of hemophilic patients undergoing CABG remain scarce.
Hypothesis
We hypothesized that patients with hemophilia undergoing CABG experience worse in-hospital outcomes compared to their non-hemophilic counterparts.
Objectives
To evaluate the impact of hemophilia on in-hospital mortality, length of stay (LOS), and hospitalization costs in patients undergoing CABG.
Methods
We conducted a retrospective cohort study using the National Inpatient Sample (NIS) from 2016 to 2022. Adult patients undergoing CABG were identified using validated ICD-10-PCS codes. Patients with a diagnosis of hemophilia were matched to non-hemophilic patients using 4:1 propensity score matching (PSM) based on sociodemographic and clinical characteristics. Covariate balance was assessed using standardized mean differences. Conditional logistic regression was used to calculate odds ratios for in-hospital mortality, generalized linear models with a gamma distribution and a log-link function were used to evaluate differences in LOS and hospitalization costs.
Results
A weighted total of 280 hospitalizations for coronary artery bypass grafting (CABG) among patients with hemophilia were identified. Following 4:1 PSM, the final cohort comprised 900 patients—180 with hemophilia and 720 without. The mean age was 63.2 years (SD 10.6), and 74.7% of patients were White. Hemophilia A accounted for 58.3% of the hemophilia patients, while Hemophilia B & C accounted for 14.4% and 27.3%, respectively. The overall in-hospital mortality rate was 4.2%. Mortality was significantly higher in the hemophilic group (10.6%) compared to the non-hemophilic group (2.6%) (OR: 4.5 (95% CI: 2.4–6.4). The median length of stay (LOS) for the entire cohort was 9 days (IQR: 8 days), and the median hospitalization cost was $46,440 (IQR: $42,654). Compared to non-hemophilic patients, those with hemophilia had a 33% longer LOS (β = 1.33 days; 95% CI: 1.18–1.49) and 62% higher hospitalization costs (β = 1.62; 95% CI: 1.43–1.84).
Conclusion
Hemophilia is linked to higher in-hospital mortality, longer stays, and greater costs in patients undergoing CABG. These findings highlight the need for enhanced perioperative care and tailored management in this high-risk group.
More abstracts on this topic:
Acoramidis Reduces All-Cause Mortality (ACM) and Cardiovascular-Related Hospitalization (CVH): Initial Outcomes From the ATTRibute-CM Open-Label Extension (OLE) Study
Judge Daniel, Masri Ahmad, Obici Laura, Poulsen Steen, Sarswat Nitasha, Shah Keyur, Soman Prem, Cao Xiaofan, Wang Kevin, Pecoraro Maria, Tamby Jean-francois, Gillmore Julian, Katz Leonid, Fox Jonathan, Maurer Mathew, Alexander Kevin, Ambardekar Amrut, Cappelli Francesco, Fontana Marianna, Garcia-pavia Pablo, Grogan Martha, Hanna Mazen
Achieving Guidelines within a 24-Hour Movement Paradigm and Risk of Cardiovascular Disease and All-Cause Mortality in United States AdultsBoudreaux Benjamin, Xu Chang, Dooley Erin, Hornikel Bjoern, Munson Alexandra, Shechter Ari, Palta Priya, Gabriel Kelley, Diaz Keith