Final ID: Mo3042
From Diagnosis to Timely Care: How Social Determinants of Health Affect Pediatric Patients with Wolff-Parkinson-White Syndrome
Abstract Body (Do not enter title and authors here): Background: Social determinants of health (SDOH) contribute to disparities in cardiovascular care and outcomes. In pediatric Wolff-Parkinson-White (WPW) syndrome, timely access to risk stratification by electrophysiology study (EPS) and possible ablation can prevent sudden cardiac death. The impact of SDOH on the management of pediatric supraventricular tachycardia has been evaluated but has not been investigated in patients with WPW specifically.
Hypothesis: We hypothesize that patients with WPW who are non-white, primarily Spanish-speaking, publicly insured, and have lower childhood opportunity index (COI) are less likely to undergo EPS and have longer waits from diagnosis to EPS.
Methods: This single-center, retrospective cohort study identified patients aged 5 to 18 years old with WPW pattern by ECG between 2014 and 2024. Patients diagnosed before 5 years of age and patients with intermittent WPW pattern were excluded. Demographic, clinical, and insurance data were extracted via chart review; census tract level COI was obtained from a validated public database. The primary outcome was the time from first diagnostic ECG to EPS. Risk stratification, accessory pathway, and procedural success data were collected from EPS reports. Odds ratio and time interval comparisons were made using 2-sample t, chi-squared, ANOVA, and Kruskal-Wallis tests.
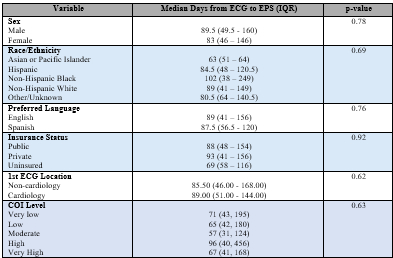
Results: Of 363 included patients, 174 (48%) are female, 222 (61%) are non-white, 58 (16%) are primarily Spanish-speaking, and 181 (50%) are publicly insured. Two hundred thirty-four (64%) underwent an EP study with a median time from ECG to EPS of 68 (IQR 41, 182) days (Table 1). Hispanic patients were less likely to undergo EPS compared to non-Hispanic whites (P=0.049), and Spanish speaking patients were less likely compared to English speaking (P=0.03). Patients with public insurance were less likely to undergo EPS compared to those with private insurance (P=0.02). Patients with lower COI levels were less likely to undergo EPS compared to those with very high COI. There was no significant difference in time from ECG to EPS or from EPS to follow-up based on demographic variables (Table 2).
Conclusion: In this diverse pediatric WPW cohort, Hispanic ethnicity, primarily Spanish-speaking, and public insurance were associated with lower likelihood of undergoing EPS. These findings identify potential barriers to timely EPS and highlight a need for targeted interventions to promote equitable care in this population.
Hypothesis: We hypothesize that patients with WPW who are non-white, primarily Spanish-speaking, publicly insured, and have lower childhood opportunity index (COI) are less likely to undergo EPS and have longer waits from diagnosis to EPS.
Methods: This single-center, retrospective cohort study identified patients aged 5 to 18 years old with WPW pattern by ECG between 2014 and 2024. Patients diagnosed before 5 years of age and patients with intermittent WPW pattern were excluded. Demographic, clinical, and insurance data were extracted via chart review; census tract level COI was obtained from a validated public database. The primary outcome was the time from first diagnostic ECG to EPS. Risk stratification, accessory pathway, and procedural success data were collected from EPS reports. Odds ratio and time interval comparisons were made using 2-sample t, chi-squared, ANOVA, and Kruskal-Wallis tests.
Results: Of 363 included patients, 174 (48%) are female, 222 (61%) are non-white, 58 (16%) are primarily Spanish-speaking, and 181 (50%) are publicly insured. Two hundred thirty-four (64%) underwent an EP study with a median time from ECG to EPS of 68 (IQR 41, 182) days (Table 1). Hispanic patients were less likely to undergo EPS compared to non-Hispanic whites (P=0.049), and Spanish speaking patients were less likely compared to English speaking (P=0.03). Patients with public insurance were less likely to undergo EPS compared to those with private insurance (P=0.02). Patients with lower COI levels were less likely to undergo EPS compared to those with very high COI. There was no significant difference in time from ECG to EPS or from EPS to follow-up based on demographic variables (Table 2).
Conclusion: In this diverse pediatric WPW cohort, Hispanic ethnicity, primarily Spanish-speaking, and public insurance were associated with lower likelihood of undergoing EPS. These findings identify potential barriers to timely EPS and highlight a need for targeted interventions to promote equitable care in this population.
More abstracts on this topic:
Acceptability and Gain of Knowledge of Community Educational Tools About Rheumatic Heart Disease Integrated With Screening In Low-Income Settings
Abrams Jessica, Nunes Maria, Diniz Marina, Fraga Lucas, Paula Luiza, Coelho Cecilia, Tacuri Chavez Luz Marina, Lemos Larissa, Correia Julliane, Ribeiro Antonio, Nascimento Bruno, Sable Craig, Spaziani Alison, Zuhlke Liesl, Cardoso Clareci, Vinhal Wanessa, Ribeiro Isabely, Oliveira Kaciane, Amaral Ingred Beatriz
Aberrant Splicing of Mitochondrial Dynamics Genes Impairs Cardiac Bioenergetics in Myotonic Dystrophy type I (DM1)Adesanya Oluwafolajimi, Nabie Pouya, Kalsotra Auinash