Final ID: Su1023
Temporal Trends in Obesity and Hypertension-Associated Mortality in the United States: Insights from CDC WONDER (1999–2020)
Abstract Body (Do not enter title and authors here):
Introduction:
Obesity is a known risk factor contributing to the development of hypertension. This study aims to identify integrated temporal trends, racial and ethnic disparities, and geographic variation in obesity-related hypertension deaths.
Methods:
We analyzed de-identified data from the CDC WONDER database (1999–2020) to examine hypertension-related mortality trends among obese U.S. adults aged 25 and older. Age-adjusted mortality rates were assessed per 100,000 population by demographics and geography, and temporal trends were evaluated using Joinpoint regression.
Results:
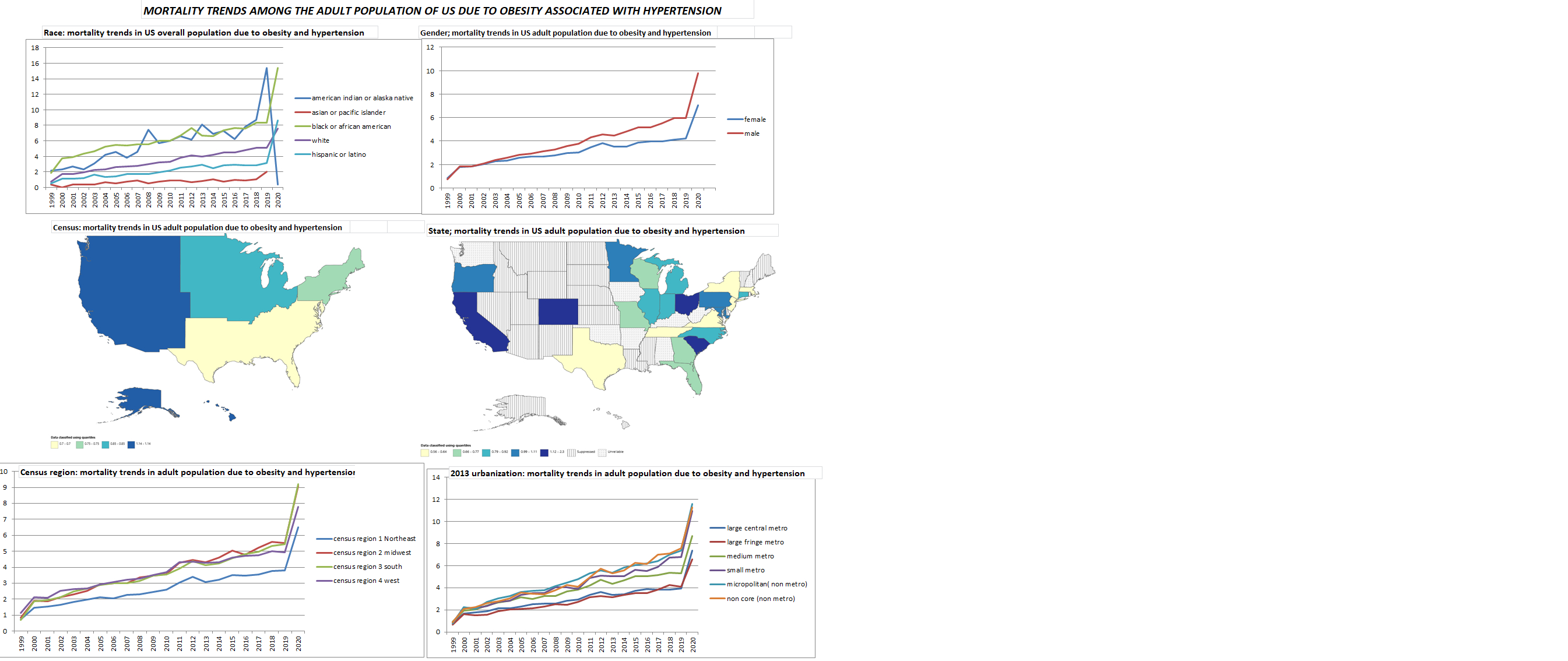
Between 1999 and 2020, 178,402 U.S. deaths were attributed to obesity and hypertension as contributing causes, with the age-adjusted mortality rate (AAMR) rising from 0.84 to 8.36 per 100,000. This reflects an overall annual percentage change (AAPC) of 7.13% (p < 0.000001) and a sharp rise from 2018 to 2020 (APC 22.95%, p = 0.0463). Males accounted for 93,806 deaths (52.58%), with an AAMR increase from 0.76 to 9.78 (AAPC 7.85%), while females had 84,596 deaths (47.42%) and an AAMR increase from 0.86 to 7.06 (AAPC 5.59%). Highest AAPCs were seen in ages 25–34 (10.63%), 35–44 (9.99%), 55–64 (9.89%), and 85+ (8.04%). By race, Whites contributed 122,976 deaths (AAPC 6.82%), Black or African Americans 31,553 (AAPC 6.29%), and Hispanics 5,314 (AAPC 9.75%, 2018–2020 APC 63.11%). American Indians or Alaska Natives had the highest AAPC (1,829 deaths, 10.51%), followed by Asians/Pacific Islanders (1,705 deaths, 7.21%). Regionally, the South had the most deaths (69,186; AAMR 0.70 to 9.21, AAPC 7.44%), with a steep post-2018 rise in the Northeast (APC 24.24%). Urban areas reported 139,918 deaths (78.43%), while rural areas had 38,484 (21.57%). California recorded the highest state count (21,496), followed by Texas (12,058); Wyoming (512) and South Dakota (587) had the lowest. These data reveal rising mortality with disparities by age, race, region, and urbanicity.
Conclusion:
HHD-related AAMR steadily rose from 1999 to 2018 and sharply increased through 2020, with higher rates in older males, the Southern and Midwest regions, and rural areas, highlighting the need for targeted public health interventions.
Introduction:
Obesity is a known risk factor contributing to the development of hypertension. This study aims to identify integrated temporal trends, racial and ethnic disparities, and geographic variation in obesity-related hypertension deaths.
Methods:
We analyzed de-identified data from the CDC WONDER database (1999–2020) to examine hypertension-related mortality trends among obese U.S. adults aged 25 and older. Age-adjusted mortality rates were assessed per 100,000 population by demographics and geography, and temporal trends were evaluated using Joinpoint regression.
Results:
Between 1999 and 2020, 178,402 U.S. deaths were attributed to obesity and hypertension as contributing causes, with the age-adjusted mortality rate (AAMR) rising from 0.84 to 8.36 per 100,000. This reflects an overall annual percentage change (AAPC) of 7.13% (p < 0.000001) and a sharp rise from 2018 to 2020 (APC 22.95%, p = 0.0463). Males accounted for 93,806 deaths (52.58%), with an AAMR increase from 0.76 to 9.78 (AAPC 7.85%), while females had 84,596 deaths (47.42%) and an AAMR increase from 0.86 to 7.06 (AAPC 5.59%). Highest AAPCs were seen in ages 25–34 (10.63%), 35–44 (9.99%), 55–64 (9.89%), and 85+ (8.04%). By race, Whites contributed 122,976 deaths (AAPC 6.82%), Black or African Americans 31,553 (AAPC 6.29%), and Hispanics 5,314 (AAPC 9.75%, 2018–2020 APC 63.11%). American Indians or Alaska Natives had the highest AAPC (1,829 deaths, 10.51%), followed by Asians/Pacific Islanders (1,705 deaths, 7.21%). Regionally, the South had the most deaths (69,186; AAMR 0.70 to 9.21, AAPC 7.44%), with a steep post-2018 rise in the Northeast (APC 24.24%). Urban areas reported 139,918 deaths (78.43%), while rural areas had 38,484 (21.57%). California recorded the highest state count (21,496), followed by Texas (12,058); Wyoming (512) and South Dakota (587) had the lowest. These data reveal rising mortality with disparities by age, race, region, and urbanicity.
Conclusion:
HHD-related AAMR steadily rose from 1999 to 2018 and sharply increased through 2020, with higher rates in older males, the Southern and Midwest regions, and rural areas, highlighting the need for targeted public health interventions.
More abstracts on this topic:
A Clinical Trial of Healthy Food Subsidies and Behavioral Interventions to Increase Fruit and Vegetable Purchasing in an Online Store
Hua Sophia, Klaiman Tamar, Dixon Erica, Volpp Kevin, Putt Mary, Coratti Samantha, White Jenna, Hossain Mohammad, Posner Hannah, Wang Erkuan, Zhu Jingsan, John Aileen
A closed-loop system based on piezoelectric thin-film sensors and photothermal nanomaterials enables precise renal denervation for the treatment of hypertensionLiu Chengzhe, Zhou Liping, Yu Lilei